ماه: شهریور 1404
تمرین تایپ دهانگشتی فارسی تیروتیرتمرین تایپ دهانگشتی فارسی تیروتیر
تمرین تایپ فارسی آنلاین/آفلاین
تمرین تایپ انگلیسی آنلاین/آفلاین
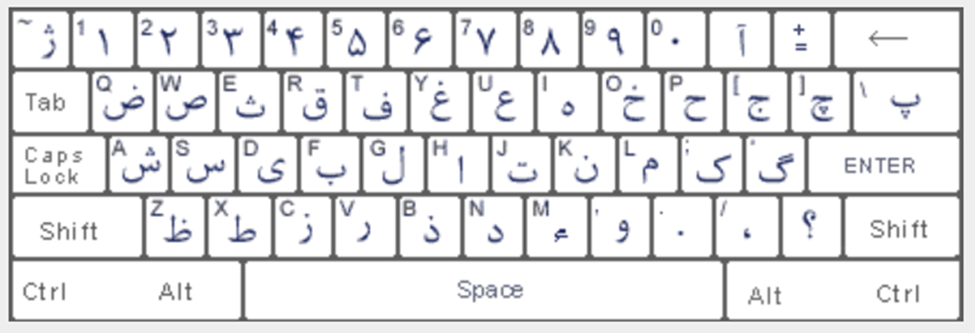

آموزش تایپ دهانگشتی فارسی
درس ۱: حروف «ت»، «ب» + کلید فاصله
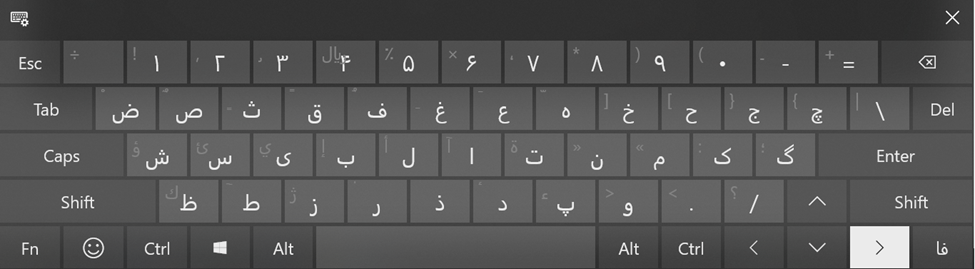
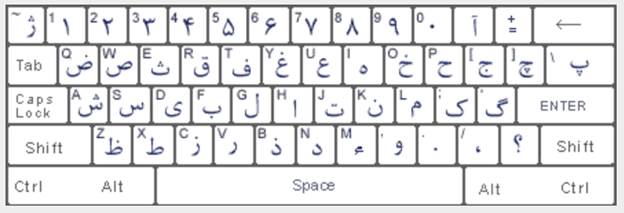
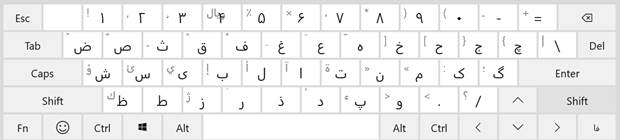
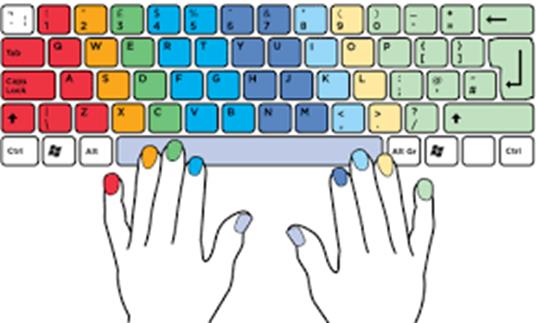
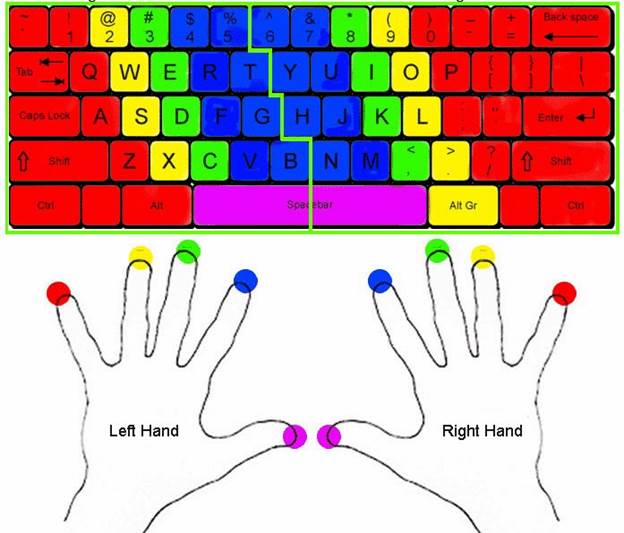
✅ یادگیری: محل قرارگیری انگشتان اشاره و شست؛ کلیدهای پایه.
🧠 نکات مهم:
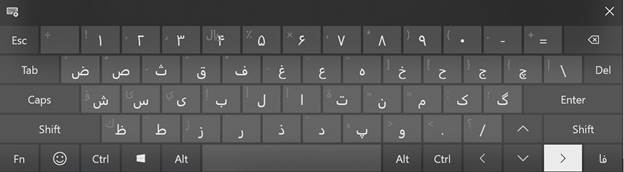
- انگشت اشاره دست چپ روی «ت»
- انگشت اشاره دست راست روی «ب»
- شستها برای زدن فاصله
✍️ تمرینها:
- ت ب ت ب ب ت ت ب
- ت ب ت ب ت ب ب ت
- تبت ببت تب تب تبتب ببتب
- چالش سرعت (۳۰ ثانیه): ت ب ت ب ت ب ت ب
درس ۲: حروف «ن» و «ی»
✅ یادگیری: استفاده از انگشتان میانی
🧠 نکات مهم:
- «ن» = انگشت میانی دست راست
- «ی» = انگشت میانی دست چپ
✍️ تمرینها:
- ن ی ن ن ی ی ن ی
- ت ب ن ی ب ن ی ت ن ت ی
- بتن یتن تبنی بیتی نیتی
- ن ی ت ب ن ت ی ب ت ب ن ی
درس ۳: حروف «م» و «س»
✅ یادگیری: استفاده از انگشتان انگشتری
🧠 نکات مهم:
- «م» = انگشت انگشتری دست راست
- «س» = انگشت انگشتری دست چپ
✍️ تمرینها:
- م س م س س م
- ت ب ن ی م س ب س ن م ت ی
- سمب نیتم یبمس تنسم
- م م س س ی ی ن ن ب ب ت ت
درس ۴: حروف «ک» و «ش»
✅ یادگیری: استفاده از انگشت کوچک دست راست و چپ
🧠 نکات مهم:
- «ک» = انگشت کوچک دست راست
- «ش» = انگشت کوچک دست چپ
✍️ تمرینها:
- ش ک ش ش ک ک ش
- ک ش م س ت ب
- کشم شتنب شمسک
- ش ک م س ن ی ب ت
درس ۵: مرور و ترکیب ۸ حرف پایه
✅ مرور: ت، ب، ن، ی، م، س، ک، ش + فاصله
✍️ تمرینها:
- ت ب ن ی م س ک ش
- شبنم، تمیش، بیکس، نیمت
- شمس تبریزی؛ بکتاش نیکسیرت
- تمرین سرعت: بنویس بدون نگاه به کیبورد (در ۱ دقیقه):
«شکستن سکوت شب، بیداری مداوم است.»
نمونه ساده ۱- آزمون نهایی آموزشگاهنمونه ساده ۱- آزمون نهایی آموزشگاه
«مفاهیم اولیه و اساسی کامپیوتر»
📝 سوالات تشریحی مفاهیم اولیه ICDL:
1. کامپیوتر را با زبان ساده تعریف کنید و مراحل اصلی کار آن را بنویسید.
2. تفاوت بین سختافزار (Hardware) و نرمافزار (Software) را توضیح دهید و برای هرکدام دو مثال بنویسید.
3. منظور از داده (Data) و اطلاعات (Information) چیست؟ با یک مثال توضیح دهید.
4. RAM و هارد دیسک چه تفاوتی با هم دارند؟ عملکرد هرکدام را توضیح دهید.
5. اینترنت چیست و چه کاربردهایی در زندگی روزمره دارد؟ حداقل ۳ مورد بنویسید.
6. سیستمعامل چیست؟ چه وظیفهای دارد و یک مثال برای آن بنویسید.
7. اگر هنگام کار با اینترنت یک ایمیل ناشناس با فایل پیوست برایتان بیاید، چه کار میکنید؟ چرا؟
8. یک مثال واقعی از کاربرد کامپیوتر در مدرسه یا خانه بنویسید و اجزای سختافزاری و نرمافزاری مورد استفاده در آن را مشخص کنید.
9. چرا داشتن رمز عبور قوی در اینترنت مهم است؟ چه نکاتی را باید برای ساخت رمز قوی رعایت کنیم؟
10. مراحل ذخیرهسازی یک فایل در کامپیوتر را به زبان ساده بنویسید (از باز کردن برنامه تا ذخیرهی فایل در فلش مموری).
🟦 بخش ویندوز (Windows) – سوالات عملی:
1. ایجاد پوشه و مدیریت فایلها
🔸 یک پوشه با نام ICDL_Practice در دسکتاپ بسازید.
🔸 داخل آن یک پوشهی دیگر به نام Documents و یک فایل متنی با نام Test.txt بسازید.
🔸 فایل را به پوشهی Documents منتقل کنید و سپس پوشهی اصلی را به فلش مموری کپی کنید.
2. شخصیسازی دسکتاپ
🔸 تصویر پسزمینه دسکتاپ را تغییر دهید و یک تصویر دلخواه از پوشهی Pictures انتخاب کنید.
🔸 رزولوشن صفحه را روی بالاترین گزینه تنظیم کنید.
3. مدیریت پنجرهها
🔸 دو پنجره باز کنید (مثلاً Notepad و File Explorer)
🔸 با استفاده از کلیدهای ترکیبی، آنها را در دو طرف صفحه قرار دهید.
🔸 بین پنجرهها جابهجا شوید و توضیح دهید از چه کلیدهایی استفاده کردید.
4. میانبرها و نوار وظیفه
🔸 یک میانبر از برنامهی Word روی دسکتاپ بسازید.
🔸 آن را به نوار وظیفه (Taskbar) سنجاق کنید.
🟨 بخش اینترنت (Internet) – سوالات عملی:
1. استفاده از موتور جستجو
🔸 با استفاده از مرورگر Chrome یا Firefox وارد سایت www.google.com شوید.
🔸 موضوع “هوش مصنوعی چیست؟” را جستجو کرده و خلاصهای از یک مقالهی مرتبط بنویسید.
2. مدیریت بوکمارکها
🔸 سایت www.wikipedia.org را باز کرده و آن را به بوکمارکهای مرورگر خود اضافه کنید.
🔸 نام آن را به “دانشنامه ویکی” تغییر دهید و در پوشهای به نام “ICDL” قرار دهید.
3. دانلود فایل و مشاهدهی مسیر ذخیره
🔸 یک فایل PDF از سایت رسمی دانلود کنید.
🔸 مسیر ذخیرهشدن فایل را مشخص کرده و آن را در پوشهی Downloads باز کنید.
4. ایمیل و پیوستها
🔸 وارد ایمیل خود شوید (مثلاً Gmail).
🔸 یک ایمیل جدید بنویسید، موضوع را “تمرین ICDL” قرار دهید و یک فایل متنی پیوست (Attach) کنید.
🔸 برای معلم یا همکلاسی خود ارسال کنید.
word
1-یک سند 5 صفحه ای ایجاد کنید که هر 3 دقیقه یکبار به طور خودکار ذخیره شود و بهصورت فقط خواندنی باز شود.
2-جدول زیر را ایجاد کنید.
| شرح | تعداد | قیمت | ||
| جمع کل | ||||
Excel
3-یک صفحه کاری ایجاد کنید و نام کاربرگ اول آن را tirotir قرار دهید و سپس قالببندی اعداد را تغییر دهید تا اعداد منفی قرمز دیده شوند.
4- جدول زیر را با فرمول مناسب ایجاد کنید و یک نمودار ستونی ۳ بعدی از آن نمایش دهید.
| نام درس | تعداد واحد | نمره | نمره باضریب |
| زبان | 2 | 15 | |
| شیمی | 3 | 16 | |
| فیزیک | 4 | 14 |
Power point
5- سه اسلاید ایجاد کنید در اسلاید اول نام خود را بصورت سه بعدی و رنگی و در اسلاید دوم یک دیاگرام و در سومی یک تصویر قرار دهید.
Access
6-جدولی ایجاد کنید که شامل فیلدهای نام و فامیلی و شماره تلفن باشد
7-برای جدول بالا گزارشی تهیه کنید که در سر صفحه آن نام شما و در پا صفحه تاریخ روز درج شده باشد.
Excel:
3-جدول زیر را با استفاده از توابع پر کنید.
A1=556 و B1=793
| کوچکتر | بزرگتر | میانگین | جمع |
4- به ستون BوCکاربرگ جاری فرمت تاریخ بدهید.
Powerpoint
5- به کلمه HAPPYبگونه ای افکت دهید که بعد از اجرای جلوه پنهان شود
6- یک ارائه کاری حاوی 7 اسلاید بسازید هریک را شماره گذاری نموده و ترتیبی دهید که به ترکیب زیر اجرا شود.(3-7-4-6-1-5-2)
Access:
7-جدولی با فیلدهای زیر را طراحی کنید و Code-pرا کلید اصلی قرار دهید
code-p(کلید اصلی –عددبصورت اتوماتیک پر شود)-نام 15 کاراکتری
8- از جدول بالا یک فرم و یک گزارش تهیه کنید.

مرور مبانی ICDLمرور مبانی ICDL
آموزشگاه هوش مصنوعی: مفاهیم اولیه کامپیوتر و سختافزار
- تعریف کامپیوتر و انواع آن
پرسش: کامپیوتر چیست و چه انواعی دارد؟
پاسخ: کامپیوتر دستگاهی است که دادهها را پردازش و نتایج را نمایش میدهد. انواع آن شامل دسکتاپ -برای کارهای ثابت-، لپتاپ -قابل حمل-، و تبلت -صفحه لمسی- است.
مثال: یک لپتاپ میتواند برای برنامهنویسی و تبلت برای خواندن کتابهای الکترونیکی استفاده شود. - شناخت اجزای اصلی کامپیوتر
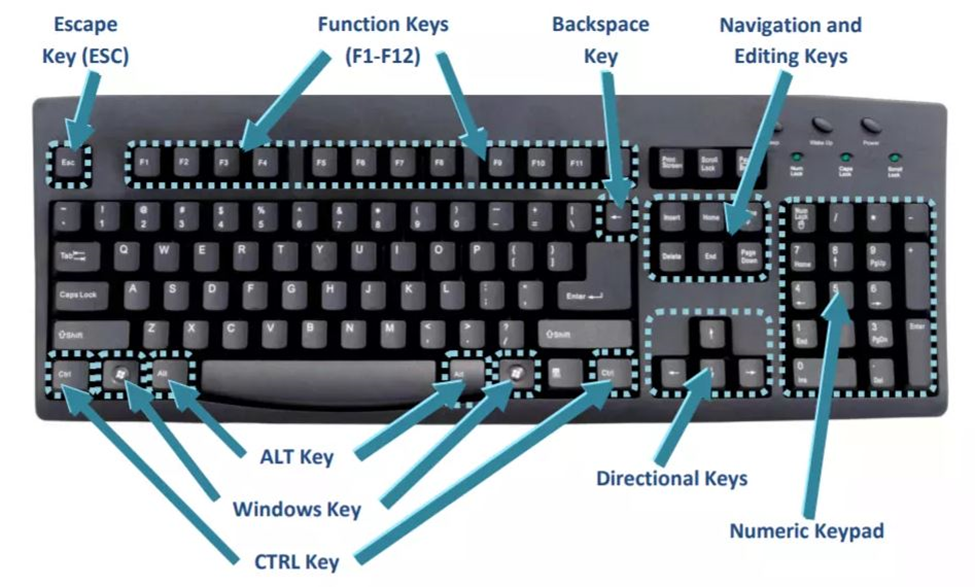
پرسش: اجزای اصلی کامپیوتر کداماند؟
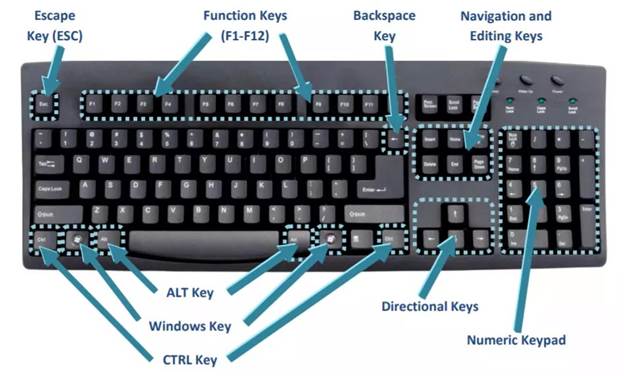
پاسخ: اجزا شامل ورودی -مانند ماوس و کیبورد-، پردازش -CPU-، خروجی -مانیتور، چاپگر-، و ذخیرهسازی -HDD/SSD- هستند.
راه عملی: کیبورد را وصل کنید و در برنامه “نوتپد” متن تایپ کنید؛ نتیجه در مانیتور نمایش داده میشود. - مفهوم سیستمعامل
پرسش: سیستمعامل چیست؟
پاسخ: سیستمعامل نرمافزاری است که بین کاربر و سختافزار واسطه میشود؛ ویندوز، لینوکس و مک از نمونهها هستند.
مثال عملی: اگر در ویندوز هستید، کلید Start را فشار دهید و نرمافزار Word را باز کنید. - تفاوت نرمافزار و سختافزار
پرسش: نرمافزار و سختافزار چه تفاوتی دارند؟
پاسخ: سختافزار اجزای فیزیکی سیستم است؛ نرمافزار برنامههایی است که روی آن اجرا میشوند.
راه عملی: ماوس را لمس کنید -سختافزار- و از مرورگر کروم برای جستجو استفاده کنید -نرمافزار-. - مدیریت فایل و پوشهها
پرسش: چگونه فایل و پوشهها را مدیریت کنیم؟
پاسخ: فایلها دادههای ذخیرهشده و پوشهها ساختاری برای مرتبسازی آنها هستند.
مثال عملی: پوشهای به نام “درس” در دسکتاپ ایجاد کنید و فایلهای متنی خود را داخل آن قرار دهید. - RAM و حافظه ذخیرهسازی
پرسش: RAM چه تفاوتی با HDD/SSD دارد؟
پاسخ: RAM حافظه موقتی است که سرعت پردازش را افزایش میدهد، ولی HDD/SSD برای ذخیرهسازی دائمی دادهها استفاده میشود.
راه عملی: مرورگر را باز کنید -RAM استفاده میشود-، سپس فایلی در هارد دیسک ذخیره کنید. - بوت شدن کامپیوتر
پرسش: بوت شدن چیست؟
پاسخ: بوت فرآیند شروع به کار کامپیوتر است که BIOS یا UEFI نقش اصلی در شناسایی سختافزارها دارد.
مثال: هنگام روشن کردن سیستم، لوگوی شرکت سازنده ظاهر میشود که نشاندهنده فرآیند بوت است. انواع دادهها
پرسش: دادهها چند نوع هستند؟
پاسخ: دادهها به متنی -docx-، صوتی -mp3-، تصویری -jpg- تقسیم میشوند.
راه عملی: یک آهنگ را در پلیر باز کنید -داده صوتی-.- درایور سختافزاری
پرسش: درایور چیست؟
پاسخ: درایور نرمافزاری است که سختافزار را برای سیستمعامل قابل استفاده میکند.
مثال عملی: اگر پرینتر کار نمیکند، بررسی کنید که درایور آن نصب شده باشد. - پورتهای ارتباطی
پرسش: پورتهای ارتباطی چه کاربردی دارند؟
پاسخ: USB برای اتصال فلش، HDMI برای نمایشگر، و Ethernet برای اتصال به شبکه استفاده میشوند.
راه عملی: فلش را به پورت USB وصل کنید و فایلها را بررسی کنید.
2- سختافزارهای اصلی کامپیوتر
- پردازنده -CPU-
پرسش: پردازنده چه نقشی در کامپیوتر دارد؟
پاسخ: CPU مغز کامپیوتر است و مسئول انجام محاسبات و اجرای دستورات است.
راه عملی: هنگام باز کردن نرمافزاری مانند فتوشاپ، CPU دادهها را پردازش کرده و نرمافزار را اجرا میکند. - کارت گرافیک -GPU-
پرسش: کارت گرافیک چه کاربردی دارد؟
پاسخ: GPU پردازش تصاویر و گرافیکهای سنگین -مانند بازی یا رندر- را انجام میدهد.
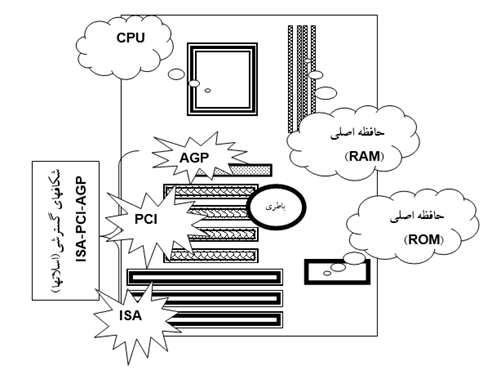
مثال عملی: هنگام بازیهای گرافیکی مانند FIFA، کارت گرافیک تصاویر را پردازش میکند. - مادربرد -Motherboard-
پرسش: مادربرد چیست؟
پاسخ: مادربرد قطعهای است که همه اجزای کامپیوتر مانند CPU، RAM، و GPU را به هم متصل میکند.
راه عملی: مادربرد را مانند مرکز کنترل کامپیوتر تصور کنید؛ تمام کابلها و قطعات به آن متصل میشوند. - حافظههای ذخیرهسازی -HDD/SSD/NVMe-
پرسش: چه تفاوتی بین HDD، SSD، و NVMe وجود دارد؟
پاسخ: HDD سرعت پایینتری دارد و مکانیکی است، SSD سریعتر و الکترونیکی است، و NVMe جدیدترین تکنولوژی با سرعت بسیار بالاست.
راه عملی: اگر بازی یا برنامهای را روی SSD نصب کنید، بسیار سریعتر اجرا میشود. - مانیتور -LCD و LED-
پرسش: مانیتور LCD با LED چه تفاوتی دارد؟
پاسخ: LED روشنایی بیشتر و مصرف کمتری دارد، اما LCD معمولاً ارزانتر است.
مثال: در مانیتور LED تصاویر روشنتر و رنگها زندهتر به نظر میرسند. - منبع تغذیه -Power Supply-
پرسش: منبع تغذیه چه وظیفهای دارد؟
پاسخ: پاور برق مورد نیاز قطعات سیستم را تأمین میکند.
راه عملی: اگر سیستم روشن نمیشود، بررسی کنید که پاور سالم باشد. - ابزارهای ورودی -Input Devices-
پرسش: ابزارهای ورودی چه هستند؟
پاسخ: ابزارهایی که داده را وارد سیستم میکنند، مانند ماوس، کیبورد و اسکنر.
راه عملی: با کیبورد متنی در Word تایپ کنید یا با ماوس روی آیکون کلیک کنید. - ابزارهای خروجی -Output Devices-
پرسش: ابزارهای خروجی چه کاربردی دارند؟
پاسخ: ابزارهایی که خروجی دادهها را نمایش میدهند، مانند مانیتور، اسپیکر، و پرینتر.
راه عملی: سندی را چاپ کنید تا خروجی آن را روی کاغذ ببینید. - قطعات خنککننده -Cooling Devices-
پرسش: قطعات خنککننده چه نقشی دارند؟
پاسخ: فن و هیتسینک دمای قطعات داخلی را کنترل و از داغ شدن بیش از حد جلوگیری میکنند.
راه عملی: هنگام اجرای بازی سنگین، صدای فن بیشتر میشود تا حرارت را کاهش دهد. - شبکههای بیسیم و کارت شبکه
پرسش: کارت شبکه چیست؟
پاسخ: کارت شبکه امکان اتصال کامپیوتر به شبکه بیسیم -Wi-Fi- را فراهم میکند.
راه عملی: Wi-Fi لپتاپ را روشن کنید و به یک شبکه متصل شوید.
3- اصول اولیه کار با کامپیوتر
- روشن و خاموش کردن صحیح
پرسش: چرا روشن و خاموش کردن صحیح مهم است؟
پاسخ: خاموش کردن ناگهانی میتواند به سیستمعامل یا سختافزار آسیب برساند.
راه عملی: برای خاموش کردن، از منوی Start گزینه Shut Down را انتخاب کنید. - اتصال لوازم جانبی
پرسش: چگونه لوازم جانبی را متصل کنیم؟
پاسخ: با استفاده از پورتهای USB، لوازم مانند ماوس، کیبورد و پرینتر به کامپیوتر متصل میشوند.
راه عملی: پرینتر را با کابل USB وصل کنید و فایل خود را چاپ کنید. - استفاده از مرورگر
پرسش: چگونه از مرورگر استفاده کنیم؟
پاسخ: مرورگرهایی مانند کروم یا فایرفاکس ابزارهایی برای دسترسی به اینترنت هستند.
راه عملی: کروم را باز کرده و آدرس www.google.com را تایپ کنید. - مدیریت برنامهها
پرسش: چگونه نرمافزار نصب یا حذف کنیم؟
پاسخ: نرمافزارها از طریق بخش “Apps” یا “Control Panel” مدیریت میشوند.
راه عملی: وارد Control Panel شوید، یک برنامه انتخاب و آن را حذف کنید. - آنتیویروس و بهروزرسانی سیستم
پرسش: چرا آنتیویروس مهم است؟
پاسخ: آنتیویروس از سیستم در برابر ویروسها و بدافزارها محافظت میکند.
راه عملی: یک نرمافزار آنتیویروس نصب کرده و سیستم را اسکن کنید. - مفهوم فایروال
پرسش: فایروال چیست؟
پاسخ: فایروال از دسترسی غیرمجاز به کامپیوتر جلوگیری میکند.
راه عملی: وارد تنظیمات ویندوز شوید و فایروال را فعال کنید. - بکاپ گرفتن از اطلاعات
پرسش: چگونه از اطلاعات بکاپ بگیریم؟
پاسخ: با استفاده از ابزارهایی مانند هارد اکسترنال یا سرویسهای ابری.
راه عملی: فایلهای مهم خود را در گوگل درایو آپلود کنید. - عیبیابی اولیه
پرسش: چگونه مشکلات ساده را حل کنیم؟
پاسخ: بررسی اتصالات، ریاستارت کردن، یا بستن برنامههای معیوب.
راه عملی: اگر سیستم هنگ کرد، دکمه Power را نگه دارید و دوباره روشن کنید. - حافظههای خارجی
پرسش: حافظههای خارجی چه کاربردی دارند؟
پاسخ: برای انتقال یا ذخیره دادهها از فلش مموری یا هارد اکسترنال استفاده میشود.
راه عملی: فایل را روی فلش ذخیره و در کامپیوتر دیگری باز کنید. - مشکلات سختافزاری رایج
پرسش: چگونه مشکلات سختافزاری را تشخیص دهیم؟
پاسخ: عدم روشن شدن سیستم ممکن است به پاور مربوط باشد؛ عدم شناسایی دستگاه به درایور.
راه عملی: اگر ماوس کار نمیکند، پورت USB را تغییر دهید یا درایور را بررسی کنید.
در سال ۲۰۲۵، شرکتهای اینتل و AMD پردازندههای جدیدی را معرفی کردهاند که عملکرد و کارایی سیستمها را بهبود میبخشند. در ادامه، به معرفی برخی از این پردازندهها و سیستمهای پیشنهادی میپردازیم.
پردازندههای جدید
اینتل:
- سری Core Ultra 200: اینتل در نمایشگاه CES 2025 از پردازندههای سری Core Ultra 200 رونمایی کرد که برای لپتاپها و سیستمهای رومیزی طراحی شدهاند. این پردازندهها با معماری بهبودیافته و مصرف انرژی کمتر، عملکرد بهتری را ارائه میدهند.
AMD:
- Ryzen 9 9955HX3D: در CES 2025، AMD از پردازنده Ryzen 9 9955HX3D رونمایی کرد که با ۱۶ هسته و ۳۲ رشته پردازشی، فرکانس ۵.۴ گیگاهرتز و ۱۴۴ مگابایت کش، عملکرد بالایی را ارائه میدهد.
سیستم پیشنهادی برای برنامهنویسی و هوش مصنوعی -بدون GPU-:
۱. سیستم اقتصادی:
- پردازنده: Intel Core i5-13500 -هستههای قدرتمند با عملکرد بالا برای پردازش چند رشتهای-.
- رم: 16 گیگابایت DDR5 -پاسخگویی سریعتر به عملیات و مدیریت چندین برنامه-.
- حافظه ذخیرهسازی: 512 گیگابایت SSD NVMe -سرعت بالا برای بوت و ذخیره پروژهها-.
- مادربرد: MSI Pro B760M-A WIFI -دارای پشتیبانی از رم DDR5 و اتصالات پیشرفته-.
- منبع تغذیه: ۶۰۰ وات -برای اطمینان از پایداری سیستم-.
کاربرد: مناسب برای کارهای روزمره برنامهنویسی و اجرای پروژههای سبک هوش مصنوعی.
۲. سیستم میانرده:
- پردازنده: AMD Ryzen 7 7700 -۸ هسته و ۱۶ رشته برای پردازشهای چندگانه-.
- رم: 32 گیگابایت DDR5 -اجرای همزمان پروژههای سنگین و ماشینهای مجازی-.
- حافظه ذخیرهسازی: 1 ترابایت SSD NVMe -فضای کافی برای دیتاستها و پروژهها-.
- مادربرد: ASUS TUF Gaming B650-PLUS -مجهز به پشتیبانی از سختافزارهای جدید-.
- منبع تغذیه: ۷۵۰ وات -برای پایداری سیستم و امکان ارتقا-.
کاربرد: مناسب برای برنامهنویسی حرفهای، مدلسازی و آموزش الگوریتمهای متوسط هوش مصنوعی.
۳. سیستم حرفهای:
- پردازنده: AMD Ryzen 9 7950X -۱۶ هسته و ۳۲ رشته با عملکرد فوقالعاده برای مدلسازی پیشرفته-.
- رم: 64 گیگابایت DDR5 -مدیریت همزمان چندین پروژه حجیم و ماشینهای مجازی-.
- حافظه ذخیرهسازی: 2 ترابایت SSD NVMe -سرعت و فضای کافی برای دیتاستهای حجیم-.
- مادربرد: Gigabyte X670E Aorus Master -با امکانات پیشرفته برای بهرهگیری از سختافزارهای مدرن-.
- منبع تغذیه: ۸۵۰ وات -قابلیت ارتقا و استفاده طولانیمدت-.
کاربرد: ایدهآل برای برنامهنویسان حرفهای و متخصصین هوش مصنوعی که با مدلهای بزرگ و پردازشهای سنگین کار میکنند.
نکات مهم:
- اگر پروژههای هوش مصنوعی شما به GPU نیاز دارد، میتوانید در آینده کارت گرافیکهای NVIDIA RTX سری ۳۰ یا ۴۰ را اضافه کنید.
- استفاده از سیستمهای SSD NVMe در تمامی پیشنهادها برای سرعت بوت و بارگذاری بسیار اهمیت دارد.
- پردازندههای Ryzen با توجه به هستههای بیشتر، برای پروژههای پردازشی و مدلسازی مناسبتر هستند.
- حتماً به تهویه مناسب کیس و استفاده از قطعات با کیفیت برای اطمینان از طول عمر سیستم توجه کنید.
آموزشگاه هوش مصنوعی
مبانی و مفاهیم اولیه کار با کامپیوتر و سختافزار
1- مفاهیم پایه کامپیوتر:
- تعریف کامپیوتر و انواع آن (دسکتاپ، لپتاپ، تبلت).
- شناخت اجزای اصلی کامپیوتر (ورودی، پردازش، خروجی، ذخیرهسازی).
- مفهوم سیستمعامل (ویندوز، لینوکس، مک).
- آشنایی با نرمافزارها و تفاوت آنها با سختافزار.
- معرفی مفهوم فایل و پوشه و نحوه مدیریت آنها.
- تفاوت بین حافظه RAM و حافظه ذخیرهسازی (HDD/SSD)
- مفهوم بوت شدن کامپیوتر و نقش BIOS/UEFI
- معرفی انواع دادهها (متنی، صوتی، تصویری).
- مفهوم درایور سختافزاری و اهمیت نصب آن.
- آشنایی با پورتهای ارتباطیUSB، HDMI، Ethernet
2- سختافزارهای اصلی کامپیوتر:
- معرفی پردازنده (CPU) و وظیفه آن.
- آشنایی با کارت گرافیک (GPU) و نقش آن در پردازش گرافیکی.
- مفهوم مادربرد (Motherboard) و ارتباط اجزا در آن.
- آشنایی با انواع حافظههای ذخیرهسازیHDD، SSD، NVMe
- تفاوت میان مانیتور LCD و LED
- کارکرد منبع تغذیه (Power Supply) و نحوه تأمین برق اجزا.
- معرفی ابزارهای ورودی: ماوس، کیبورد، اسکنر.
- آشنایی با ابزارهای خروجی: پرینتر، اسپیکر.
- آشنایی با قطعات خنککننده (فن، هیتسینک).
- معرفی شبکههای بیسیم و کارتهای شبکه (Wi-Fi Adapter)
3- اصول اولیه کار با کامپیوتر:
- روشن و خاموش کردن صحیح کامپیوتر.
- اتصال و نصب لوازم جانبی (پرینتر، ماوس، کیبورد).
- نحوه استفاده از مرورگر برای دسترسی به اینترنت.
- مدیریت برنامهها (نصب و حذف نرمافزار).
- اهمیت آنتیویروس و بهروزرسانی سیستم.
- مفهوم فایروال و نقش آن در امنیت کامپیوتر.
- بکاپ گرفتن از اطلاعات شخصی.
- اصول عیبیابی اولیه (ریاستارت، بررسی اتصالات).
- نحوه استفاده از حافظههای خارجی (فلش مموری، هارد اکسترنال).
- شناسایی مشکلات سختافزاری رایج (مانند روشن نشدن سیستم یا عدم شناسایی دستگاهها).
مرور پاورپوینت و عملیمرور پاورپوینت و عملی
۳۰ مورد برای پاورپوینت:
- ایجاد یک اسلاید جدید
انتخاب تب Home –> New Slide –> انتخاب نوع اسلاید. - افزودن متن به اسلاید
کلیک روی جعبه متنی و تایپ متن. - افزودن تصویر به اسلاید
انتخاب تب Insert –> Pictures –> انتخاب تصویر از محل ذخیره. - استفاده از قالب آماده (Theme)
انتخاب تب Design –> انتخاب قالب (Theme) از گالری. - انتخاب طرحبندی (Layout) اسلاید
انتخاب اسلاید –> انتخاب تب Home –> Layout –> انتخاب طرحبندی. - انتقال بین اسلایدها با استفاده از انیمیشنها
انتخاب اسلاید –> انتخاب تب Transitions –> انتخاب نوع انتقال. - افزودن لینکهای اینترنتی به اسلاید
انتخاب متن یا تصویر –> راستکلیک –> Hyperlink –> وارد کردن URL. - استفاده از انیمیشن برای اشیاء
انتخاب شیء –> انتخاب تب Animations –> انتخاب نوع انیمیشن. - ایجاد نمودار در اسلاید
انتخاب تب Insert –> Chart –> انتخاب نوع نمودار و وارد کردن دادهها. - ایجاد جعبه متن در اسلاید
انتخاب تب Insert –> Text Box –> تایپ متن در جعبه. - افزودن ویدیو به اسلاید
انتخاب تب Insert –> Video –> انتخاب ویدیو از فایل یا آنلاین. - استفاده از SmartArt در پاورپوینت
انتخاب تب Insert –> SmartArt –> انتخاب نوع SmartArt.
- تنظیم زمان برای هر اسلاید
انتخاب تب Transitions –> مدت زمان برای نمایش اسلاید را وارد کنید. - ایجاد افکت برای اشیاء هنگام ورود به اسلاید
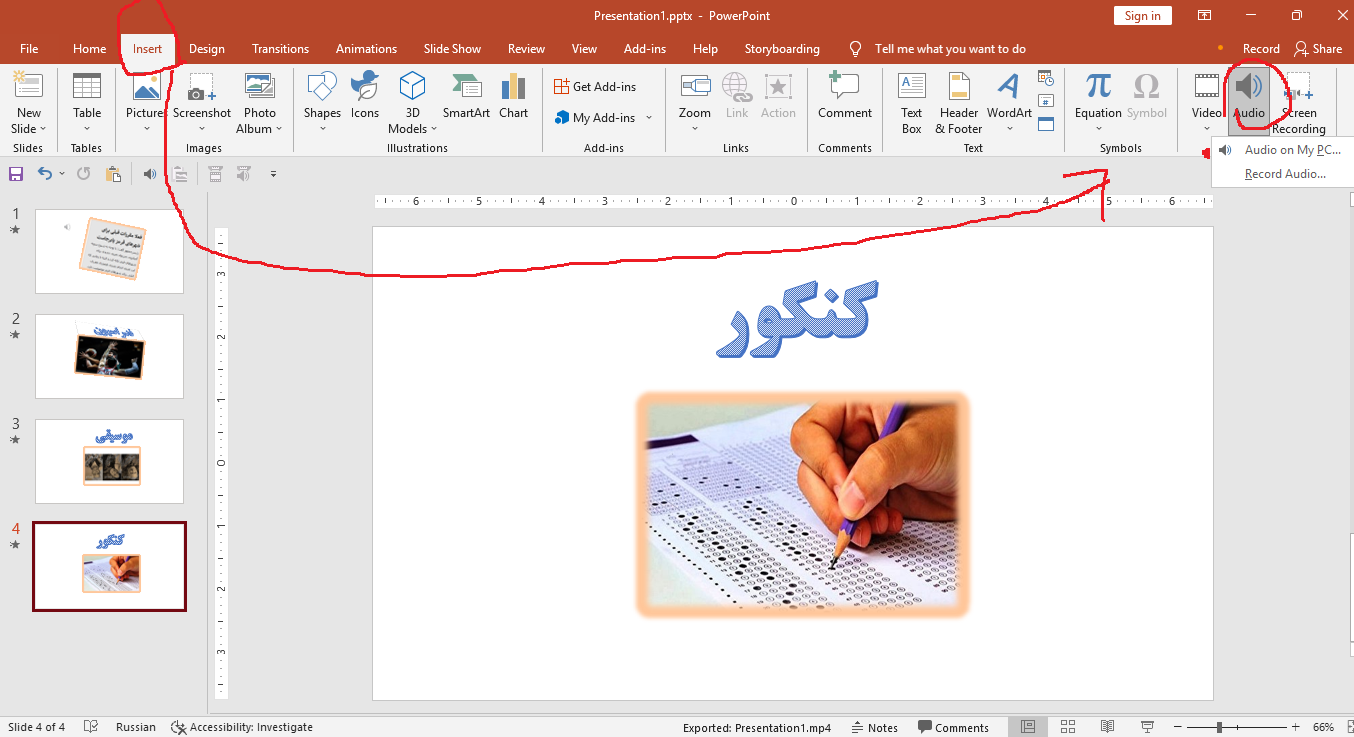
انتخاب شیء –> انتخاب تب Animations –> انتخاب نوع انیمیشن ورود. - افزودن صدا به اسلاید
انتخاب تب Insert –> Audio –> انتخاب منبع صدا. - تنظیم یک اسلاید به عنوان اسلاید عنوان
انتخاب اسلاید اول –> انتخاب تب Home –> Layout –> انتخاب Title Slide. - ایجاد فهرست مطالب در پاورپوینت
استفاده از جعبه متن و Bullet Points برای ایجاد فهرست. - استفاده از قابلیت Slide Master برای تنظیمات کلی
انتخاب تب View –> Slide Master –> ویرایش قالبهای اسلاید.
- ایجاد جدول در اسلاید
انتخاب تب Insert –> Table –> انتخاب تعداد ردیف و ستون. - افزودن حاشیه به اسلاید
انتخاب تب Design –> Page Borders –> انتخاب حاشیه برای اسلاید. - نمایش اسلاید به صورت Full Screen
فشار دادن F5 یا انتخاب تب Slide Show –> From Beginning. - افزودن انیمیشن به متن
انتخاب متن –> انتخاب تب Animations –> انتخاب نوع انیمیشن. - ذخیره پاورپوینت به صورت PDF
انتخاب تب File –> Save As –> انتخاب PDF. - استفاده از قابلیت Slide Show برای تمرین
انتخاب تب Slide Show –> Rehearse Timings. - افزودن پاورقی به اسلاید
انتخاب تب Insert –> Footer –> وارد کردن متن پاورقی. - پیدا کردن اسلاید خاص با استفاده از جستجو
فشار دادن Ctrl+F و تایپ عنوان اسلاید برای جستجو. - تنظیمات چاپ برای اسلاید
انتخاب تب File –> Print –> تنظیمات چاپ (اسلایدهای تک یا چندگانه). - استفاده از لایهها برای ترتیب اشیاء
راستکلیک روی شیء –> Send to Back یا Bring to Front. - درج کد QR به اسلاید
انتخاب تب Insert –> QR Code –> وارد کردن URL یا اطلاعات. - ایجاد لینک به اسلاید دیگر در پاورپوینت
انتخاب متن یا تصویر –> راستکلیک –> Hyperlink –> انتخاب اسلاید مقصد.
آموزشگاه هوش مصنوعی
مایکروسافت پاورپوینت:
- ایجاد یک فایل پاورپوینت جدید.
- ذخیره فایل با فرمت .pptx یا .pdf.
- افزودن اسلاید جدید با قالببندی مختلف.
- تغییر پسزمینه اسلایدها.
- اضافه کردن متن و تنظیم فونت (نوع، اندازه، رنگ).
- اعمال قالبهای پیشفرض (Themes).
- تغییر ترتیب اسلایدها.
- استفاده از Slide Layouts برای تنظیم متن و تصاویر.
- اضافه کردن تصاویر به اسلاید.
- افزودن ویدیو به اسلاید.
- درج لینک (Hyperlink) به یک اسلاید دیگر یا وبسایت.
- استفاده از Bullet و Number برای لیستها.
- تنظیم افکتهای ساده برای انتقال بین اسلایدها (Transitions).
- استفاده از جدول برای سازماندهی دادهها.
- ایجاد و تنظیم نمودار (Chart).
- استفاده از Shapes برای طراحی ساده.
- تغییر رنگ و تنظیمات خطوط (Outline).
- کار با ابزار Align برای تنظیم دقیق المانها.
- افزودن آیکونها و نمادها (Icons).
- تغییر اندازه و مکان اشیاء در اسلایدها.
متوسط
- استفاده از SmartArt برای نمایش اطلاعات بصری.
- اضافه کردن افکتهای حرکتی به متن یا تصاویر (Animations).
- تنظیم زمانبندی انیمیشنها (Animation Pane).
- ضبط صدای گوینده برای اسلایدها.
- اضافه کردن Header و Footer به اسلایدها.
- استفاده از ابزار Master Slide برای تنظیم قالب کلی.
- طراحی اسلایدهای چندرسانهای (ترکیب متن، تصویر، و صدا).
- استفاده از ابزار Format Painter برای کپی تنظیمات.
- افزودن یادداشت (Notes) برای هر اسلاید.
- تنظیم اندازه اسلاید (16:9 یا 4:3).
تمرین عملی اکسل و مرورتمرین عملی اکسل و مرور
تمرین عملی اکسل
تمرین: مدیریت فروش محصولات
فرض کنید یک فروشگاه سه محصول مختلف میفروشد و دادههای فروش ماهانهی آنها به شرح زیر است:
| ماه | kala1 (تعداد) | kala2 (تعداد) | kala3 (تعداد) |
| ژانویه | 120 | 80 | 150 |
| فوریه | 100 | 90 | 200 |
| مارس | 140 | 110 | 170 |
| آوریل | 130 | 100 | 180 |
اهداف تمرین:
- محاسبه مجموع فروش هر محصول.
- محاسبه میانگین فروش ماهانه برای هر محصول.
- شناسایی پرفروشترین محصول هر ماه.
- ایجاد نمودار فروش ماهانه برای هر محصول.
گام ۱: ورود دادهها
ابتدا دادههای جدول بالا را در اکسل وارد کنید.
گام ۲: محاسبه مجموع فروش هر محصول
- در سلول E2، فرمول زیر را وارد کنید:
=SUM(B2:B5)
این فرمول مجموع فروش kala1 را محاسبه میکند. آن را به سلولهای دیگر E3 و E4 کپی کنید تا مجموع فروش برای kala2 و ۳ نیز محاسبه شود.
گام ۳: محاسبه میانگین فروش ماهانه
- در سلول F2، فرمول زیر را وارد کنید:
=AVERAGE(B2:B5)
این فرمول میانگین فروش kala1 را محاسبه میکند. آن را به سلولهای دیگر F3 و F4 کپی کنید تا میانگین فروش برای kala2 و ۳ نیز محاسبه شود.
گام ۴: شناسایی پرفروشترین محصول هر ماه
- در سلول G2، فرمول زیر را وارد کنید:
=IF(MAX(B2:D2)=B2,”kala1″,IF(MAX(B2:D2)=C2,”kala2″,”kala3″))
این فرمول بررسی میکند که کدام محصول بیشترین فروش را در ژانویه داشته است. آن را به سایر سلولهای ستون G کپی کنید تا برای سایر ماهها نیز محاسبه شود.
گام ۵: ایجاد نمودار فروش ماهانه
- دادههای ستونهای A تا D (ماه و تعداد فروش محصولات) را انتخاب کنید.
- به بخش Insert بروید و نمودار Column Chart یا Line Chart را انتخاب کنید.
- نمودار را به دلخواه ویرایش کنید (اضافه کردن عنوان، رنگها و …).
\
چند تمرین دیگر برای تقویت مهارت کار با اکسل
تمرین ۱: مدیریت هزینهها و درآمدها
دادهها:
| ماه | هزینه (تومان) | درآمد (تومان) |
| ژانویه | 5000000 | 7000000 |
| فوریه | 4000000 | 6000000 |
| مارس | 4500000 | 7500000 |
| آوریل | 6000000 | 8000000 |
اهداف تمرین:
- محاسبه سود خالص هر ماه (درآمد – هزینه) در ستون جدید.
- شناسایی ماهی که بیشترین سود خالص را داشته است.
- محاسبه مجموع هزینهها و درآمدها در پایان جدول.
- ایجاد نمودار خطی برای نمایش سود خالص ماهانه.
گامها:
- در ستون D، فرمول زیر را وارد کنید:
=C2-B2
و آن را برای سایر ماهها کپی کنید.
- برای شناسایی ماه با بیشترین سود خالص، از تابع MAX و MATCH استفاده کنید:
=INDEX(A2:A5,MATCH(MAX(D2:D5),D2:D5,0))
- مجموع هزینهها و درآمدها را با تابع SUM در زیر ستونها محاسبه کنید.
- نمودار خطی برای ستونهای A و D ایجاد کنید.
تمرین ۲: نمرات دانشآموزان
دادهها:
| نام دانشآموز | ریاضی | علوم | زبان انگلیسی | معدل |
| علی | 18 | 15 | 17 | |
| رضا | 12 | 14 | 16 | |
| سارا | 20 | 19 | 18 | |
| مریم | 14 | 13 | 15 |
اهداف تمرین:
- محاسبه معدل هر دانشآموز (میانگین نمرات در ستون معدل).
- شناسایی دانشآموزی که بالاترین معدل را دارد.
- هایلایت کردن نمرات زیر 12 با استفاده از Conditional Formatting
گامها:
- در ستون E، فرمول زیر را وارد کنید:
=AVERAGE(B2:D2)
و آن را برای سایر دانشآموزان کپی کنید.
- برای شناسایی بالاترین معدل:
=INDEX(A2:A5,MATCH(MAX(E2:E5),E2:E5,0))
- از منوی Conditional Formatting گزینه Highlight Cell Rules را انتخاب کرده و نمرات زیر 12 را قرمز کنید.
تمرین ۳: مدیریت انبار
دادهها:
| محصول | تعداد موجودی | قیمت واحد (تومان) | ارزش کل (تومان) |
| kala1 | 50 | 20000 | |
| kala2 | 30 | 50000 | |
| kala3 | 100 | 15000 | |
| محصول ۴ | 20 | 70000 |
اهداف تمرین:
- محاسبه ارزش کل موجودی برای هر محصول (تعداد × قیمت واحد).
- محاسبه مجموع ارزش کل موجودی انبار.
- شناسایی محصولی که بیشترین ارزش را دارد.
گامها:
- در ستون D، فرمول زیر را وارد کنید:
=B2*C2
و آن را برای سایر ردیفها کپی کنید.
- برای مجموع ارزش کل:
=SUM(D2:D5)
- برای شناسایی محصول با بیشترین ارزش:
=INDEX(A2:A5,MATCH(MAX(D2:D5),D2:D5,0))
تمرین ۴: تحلیل دادههای فروش
دادهها:
| ماه | محصول A | محصول B | محصول C |
| ژانویه | 100 | 150 | 200 |
| فوریه | 120 | 130 | 180 |
| مارس | 110 | 140 | 220 |
| آوریل | 130 | 160 | 210 |
اهداف تمرین:
- محاسبه مجموع فروش هر ماه.
- محاسبه درصد سهم هر محصول از کل فروش هر ماه.
- ایجاد نمودار دایرهای برای نمایش درصد سهم محصولات در ماه ژانویه.
گامها:
- در ستون D، مجموع فروش هر ماه را محاسبه کنید:
=SUM(B2:D2)
- در ستونهای جدیدE، F، G، درصد سهم هر محصول را محاسبه کنید:
=B2/$D2*100
برای سایر ستونها نیز این فرمول را اعمال کنید.
- برای نمودار دایرهای، دادههای ماه ژانویه را انتخاب کنید و از Insert > Pie Chart استفاده کنید.
تمرین ۵: تحلیل زمانی دادهها
دادهها:
| تاریخ | فروش (تومان) |
| 2025-01-01 | 5000000 |
| 2025-01-02 | 6000000 |
| 2025-01-03 | 5500000 |
| 2025-01-04 | 7000000 |
اهداف تمرین:
- محاسبه مجموع فروش.
- محاسبه میانگین فروش روزانه.
- ایجاد نمودار خطی برای نمایش روند فروش.
گامها:
- مجموع فروش را با تابع SUM محاسبه کنید.
- میانگین فروش را با تابع AVERAGE به دست آورید.
- نمودار خطی برای ستونهای A و B ایجاد کنید.
- ایجاد یک شیت جدید
کلیک روی تب + در پایین صفحه یا فشار دادن Shift+F11. - وارد کردن داده به یک سلول
انتخاب سلول –> تایپ داده مورد نظر. - انتخاب چندین سلول
کلیک و کشیدن موس یا استفاده از Shift + جهتنما. - کپی کردن دادهها
انتخاب سلولها –> Ctrl+C –> انتخاب محل جدید –> Ctrl+V. - انتقال دادهها به محل جدید
انتخاب سلولها –> Ctrl+X –> انتخاب محل جدید –> Ctrl+V. - حذف دادهها از یک سلول
انتخاب سلول –> Delete. - استفاده از فرمول جمع (SUM)
انتخاب سلول –> تایپ =SUM(A1:A5) –> Enter. - استفاده از فرمول میانگین (AVERAGE)
انتخاب سلول –> تایپ =AVERAGE(A1:A5) –> Enter. - استفاده از فرمول شمارش (COUNT)
انتخاب سلول –> تایپ =COUNT(A1:A5) –> Enter. - ایجاد یک جدول (Table)
انتخاب دادهها –> انتخاب تب Insert –> Table. - ایجاد نمودار (Chart)
انتخاب دادهها –> انتخاب تب Insert –> انتخاب نوع نمودار. - افزودن فیلتر به دادهها
انتخاب دادهها –> انتخاب تب Data –> Filter. - مرتبسازی دادهها به ترتیب صعودی یا نزولی
انتخاب دادهها –> انتخاب تب Data –> Sort –> انتخاب گزینه مرتبسازی. - یافتن دادهها با استفاده از جستجو
فشار دادن Ctrl+F –> تایپ کلمه یا عدد مورد نظر. - فرمت کردن سلولها به عنوان درصد
انتخاب سلول –> راستکلیک –> Format Cells –> Percentage. - ایجاد یک سلول با تاریخ جاری
انتخاب سلول –> تایپ =TODAY() –> Enter. - ایجاد یک سلول با ساعت جاری
انتخاب سلول –> تایپ =NOW() –> Enter. - اعمال فرمت پولی (Currency) به سلولها
انتخاب سلول –> راستکلیک –> Format Cells –> Currency. - استفاده از شرطی (Conditional Formatting)
انتخاب دادهها –> انتخاب تب Home –> Conditional Formatting –> انتخاب نوع فرمت. - قرار دادن رنگ پسزمینه به سلولها
انتخاب سلولها –> راستکلیک –> Format Cells –> Fill –> انتخاب رنگ. - چرخاندن متن در یک سلول
انتخاب سلول –> راستکلیک –> Format Cells –> Alignment –> انتخاب Rotate Text. - محاسبه بیشترین مقدار (MAX)
انتخاب سلول –> تایپ =MAX(A1:A5) –> Enter. - فرمول جمع
=A2+A3
فرمول معدل:
=(A2+A3+A4)/3
- محاسبه کمترین مقدار (MIN)
انتخاب سلول –> تایپ =MIN(A1:A5) –> Enter. - استفاده از توابع IF
انتخاب سلول –> تایپ =IF(A1>10, “Yes”, “No”) –> Enter. - مخفی کردن ستون یا ردیف
راستکلیک روی شماره ستون یا ردیف –> Hide. - افزودن حاشیه به سلولها
انتخاب سلولها –> راستکلیک –> Format Cells –> Border –> انتخاب نوع حاشیه. - ایجاد یک پیوند (Hyperlink)
انتخاب سلول –> راستکلیک –> Hyperlink –> وارد کردن URL. - ایجاد یک فیلد جستجو با استفاده از VLOOKUP
انتخاب سلول –> تایپ =VLOOKUP(A1, B1:C5, 2, FALSE) –> Enter. - استفاده از فرمول CONCATENATE برای ترکیب متن
انتخاب سلول –> تایپ =CONCATENATE(A1, ” “, B1) –> Enter. - درج یک کاما در فرمول برای تعداد هزارگان
انتخاب سلول –> راستکلیک –> Format Cells –> Number –> انتخاب Thousands Separator. - تغییر عرض ستونها
انتخاب ستونها –> راستکلیک –> Column Width –> وارد کردن اندازه جدید. - تغییر ارتفاع ردیفها
انتخاب ردیفها –> راستکلیک –> Row Height –> وارد کردن ارتفاع جدید. - قرار دادن شماره ردیفها در یک ستون
تایپ=ROW()در سلول اول و کشیدن آن به پایین. - ایجاد یک سلول با محاسبه مجموع (SUM) از سلولهای مختلف
انتخاب سلول –> تایپ=SUM(A1, B2, C3)–> Enter. - استفاده از تابع COUNTA برای شمارش تعداد سلولهای غیرخالی
انتخاب سلول –> تایپ=COUNTA(A1:A5)–> Enter. - انتخاب سلول با استفاده از Go To
فشار دادن Ctrl+G –> وارد کردن مرجع سلول (مثلا A1) –> Enter. - مخفی کردن شیتها
راستکلیک روی نام شیت –> Hide. - نمایش شیتهای مخفی شده
راستکلیک روی هر شیت –> Unhide –> انتخاب شیت مخفی. - محاسبه تعداد کاراکتر در یک سلول با استفاده از LEN
انتخاب سلول –> تایپ=LEN(A1)–> Enter. - ایجاد تاریخ و زمان در یک سلول
تایپ=NOW()در سلول –> Enter. - استفاده از TEXT برای تغییر فرمت تاریخ
تایپ=TEXT(A1, "mm/dd/yyyy")–> Enter. - جدا کردن متن در یک سلول با استفاده از TEXT TO COLUMNS
انتخاب سلول –> انتخاب تب Data –> Text to Columns –> انتخاب Delimited. - ساخت یک نمودار با دادههای انتخابی
انتخاب دادهها –> انتخاب تب Insert –> انتخاب نوع نمودار. - درج یک خط افقی در بین دادهها
انتخاب یک سلول –> تایپ=REPT("-", 50)–> Enter. - ترتیب دادهها به صورت صعودی یا نزولی
انتخاب دادهها –> انتخاب تب Data –> Sort –> انتخاب گزینه مورد نظر. - استفاده از تابع IF برای مقایسه مقادیر
تایپ=IF(A1>10, "Yes", "No")–> Enter. - برجسته کردن سلولهایی که شرایط خاصی دارند (Conditional Formatting)
انتخاب دادهها –> انتخاب تب Home –> Conditional Formatting –> انتخاب نوع شرط. - استفاده از فرمول SUBTOTAL برای محاسبات با فیلترها
انتخاب سلول –> تایپ=SUBTOTAL(9, A1:A5)–> Enter. - پیدا کردن اولین یا آخرین سلول در یک ستون با استفاده از INDEX
تایپ=INDEX(A1:A5, 1)برای اولین یا=INDEX(A1:A5, COUNTA(A1:A5))برای آخرین. - ایجاد یک فیلتر برای دادهها
انتخاب دادهها –> انتخاب تب Data –> Filter –> فعال کردن فیلتر.
۴- واژهپرداز Word۴- واژهپرداز Word
Microsoft Word
مؤلفين:
داريوش عليپور، مينوش حيدري
آموزشگاه هوش مصنوعی
tirotir.ir
فهرست
1-1 آشنايی با تعريف واژه پرداز 9
1-2 آشنايي با اجراي برنامه Word.. 9
1-3 آشنايی با محيط اصلي Microsoft Word.. 9
1-3-3 نوارهاي ابزارToolbars. 10
1-3-3-1 نوار ابزار استاندارد. 10
1-3-5 محيط تايپ (Text Area). 12
1-3-6 نوار وضعيت (Status Bar). 12
1-3-7 نوارهاي پيمايش افقي(Horizontal) و عمودي(Vertical). 12
1-4 آشنايي با ايجاد سند جديد. 13
1-5 آشنايي با چگونگی باز نمودن سند موجود. 13
1-6 آشنايي با ذخيره کردن سند فعلي با فرمتهای گوناگون. 14
1-7 آشنايی با اصول ويرايش متن.. 14
1-7-1 آشنايي با چگونگی انتخاب متن (Highlighting Text ). 15
1-7-2 شناسايي اصول کپی، بريدن، چسباندن و حذف متن.. 16
1-7-7 رنگ زمينه قلم (Highlight). 17
1-7-8 رنگ قلم (Font Color). 17
1-7-9 آشنايي با استفاده از دستور برگشت… 17
1-7-10 آشنايي با نحوه ضخيم و پررنگ کردن متن انتخاب شده Bold)). 17
1-7-11 آشنايي با نحوه زير خط دار کردن متن انتخاب شده (Underline). 17
1-7-12 آشنايي با نحوه مايل و ايتاليك کردن متن انتخاب شده (Italic). 17
1-7-13 آشنايي با ابزار چيدمان.. 18
1-8 شناسايي اصول تنظيم قلم و اندازه قلم. 18
1-8-2 برگه Character Spacing (برگه دوم از كادر Font). 19
1-8-3 برگه Text Effects (برگه سوم از كادر Font). 20
1-9 آشنايي با چگونگی استفاده از پيوند در مکان مناسب(Hyperlink) 20
1-10 آشنايي با حالتهای مختلف نمايش سندDocument View.. 20
1-11 آشنايي با ابزارهای بزرگ نمايي و کوچک نمايي سند(Zoom) 21
1-12 آشنايي با چگونگی تايپ يک پاراگراف جديد. 21
1-13 فرو رفتگی و بيرون رفتگی ابتدای يك پاراگراف.. 22
1-14 آشنايي با تغيير فاصله بين سطرها Line Spacing) ) 22
1-15 آشنايي با درج صفحه گسترده در سند. 23
1-16 شناسايي اصول ايجاد جدول و عمليات بر روی آن. 23
1-16-1 نمايش نوار ابزار جدولها و كادرها 24
1-16-3 ادغام چند خانه از جدول در يک خانه. 26
1-16-5 تايپ عمودی در خانه های جدول.. 26
1-16-7 اضافه کردن ستون و سطر جديد.. 26
1-17 آشنايي با چگونگی کار دکمه های نوار ابزار ترسيمات (Drawing) 27
1-18 آشنايي با چگونگی استفاده از برنامه راهنما (Help) 28
1-19 آشنايي با چگونگی استفاده از ابزار بررسی کننده املايي و دستوری.. 30
1-20 آشنايي با استفاده از فهرستهای اعداد و علامتها 31
1-21 آشنايي با چگونگی ايجاد صفحات جديد در سند فعلی.. 34
1-22 آشنايي با اضافه کردن سرصفحه و پاورقی (Header And Footer) 34
1-23 آشنايي با شماره بندي صفحات سند. 35
1-24 آشنايي با قرار دادن كاراكترهاي ويژه در سند. 36
1-25 آشنايي با درج تصوير، نمودار و اشياء ديگر. 36
1-26 آشنايي با چگونگی تنظيم قرار گرفتن متن و تصوير. 37
1-27 آشنايي با اضافه کردن کادر به سند و تنظيمات كادرها و سايه ها 37
1-28 آشنايي با استفاده از مجموعه های مختلف چند فاصله (Tab) 38
1-29 آشنايي با پيش نمايش چاپ (Print Priew) 40
1-30 آشنايي با تنظيمات صفحه و حاشيه سند. 41
1-30-4 شناسايي اصول چاپ سند (Print). 43
1-30-4-1 آشنايي با گزينه های اصلی چاپ… 43
1-31 شناسايي اصول انتخاب الگوی مناسب (Template) 45
1-32 آشنايي با بکار بردن يک شيوه يا سبك (Style) 45
1-33 آشنايي با اصول عمليات ادغام پستي (Mail Merge) 46
1-35 پاكت نامه ها و برچسب ها(Envelopes And Labels ) 52
1-36 شمارش كلمات(Word Count…) 52
1-38 ايجاد يادداشت(Comment) 52
1-39 ستون بندي متن (Columns) 52
1-40 انتقال قالب بندي(Format Painter) 53
1-42 برنامه جايگزينی کلمات (Replace ) 54
1-43 آشنايي با نحوه جابجايي سريع مکان نما در سند (Go To) 55
1-45 برخي كليدهاي ميان بر مربوط به برنامه Microsoft Office Word.. 57
“براي اين كه حدود امكانات را كشف كنيم، تنها راهش اين است كه آنها را پشت سر گذاشته و به قلمرو غيرممكن ها وارد شويم” آرتور سي كلارك
مقدمه
گواهينامه بين المللی کاربری کامپيوتر International Computer Driving Licence)) دوره استانداردي مي باشد كه در بيش از 35 كشور جهان به رسميت شناخته شده و دارندگان اين مدرك، جهت اشتغال و كاريابي در اولويت قرار مي گيرند. هدف ICDL ارتقاي سطح تواناييهاي كاربران در فن آوري اطلاعات و بالا بردن سطح كيفي و كمي کارايي در ادارات، موسسات و شركتها مي باشد. مدرک ICDL نشانه داشتن دانش فني لازم و توانمندی در مهارتهای کامپيوتری مي باشد. بديهي است كه اخذ مدرک ICDL به کار فرمايان و مديران مراكز كاري اطمينان می دهد که اطلاعات و دانش دارندگان اين مدرک کاملا بروز و معتبر است .
مهارتهای ICDL عبارتند از :مفاهيم اوليه فن آوری اطلاعات(IT) – استفاده ازکامپيوترومديريت فايلها – اطلاعات و ارتباطات( اينترنت و پست الکترونيک ) – واژه پرداز Word – صفحه گسترده Excel – اسلايدسازي و نمايش تبليغاتیPowerpoint – پايگاه داده Access
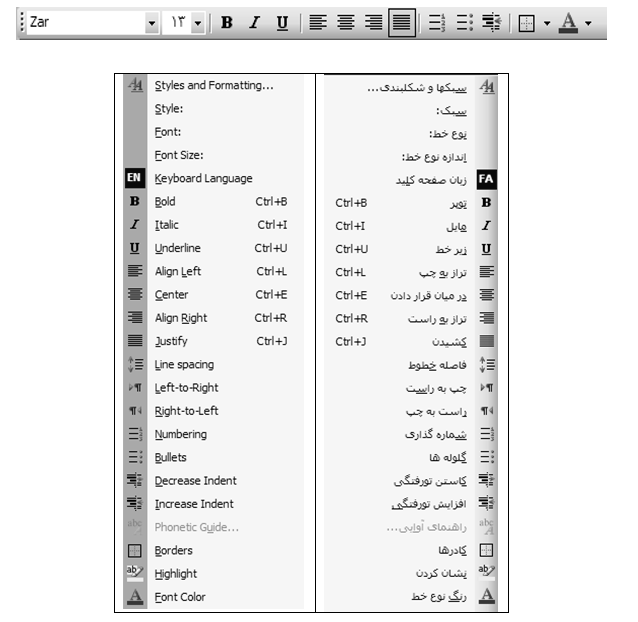
در اين كتاب، مطابق جديدترين استانداردهاي فني و حرفه اي، مهارت Word كه بخشي از مهارتهاي درجه يكِ اين دوره ميباشد، تقديم شده است. در اكثر ادارهها، سازمانها و شركتها، از اين مجموعه به عنوان يك ابزار اصلي استفاده ميشود، در بين كاربران خانگي هم طرفداران زيادي دارد. تمامي محصولات Office اين قابليت را دارند كه فايلهاي خود را به قالب HTML (فرمت فايلهاي اينترنت) درآورند تا در محيط وب نيز قابل نمايش باشند. اين مجموعه نرم افزاري، مورد استفاده ميليونها كاربر در كشورهاي مختلف بوده و آشنايي با برنامه هاي آن از ضروريات محسوب مي گردد. در ادامه بطور مختصر به شرح اين برنامه ها می پردازيم:
– Word : برنامه مخصوص واژه پردازي مي باشد كه براي ايجاد نامه ها، گزارش ها، روزنامه ها، خبرنامه ها و آگهي ها ايده آل است. برخی از قابليتهای آن عبارتند از: پاراگرافبندي، صفحهآرايي، ساختن جدول، ايجاد سرصفحه و پاصفحه (Header and Footer) ، تصحيح املايي و دستوري جمله ها .
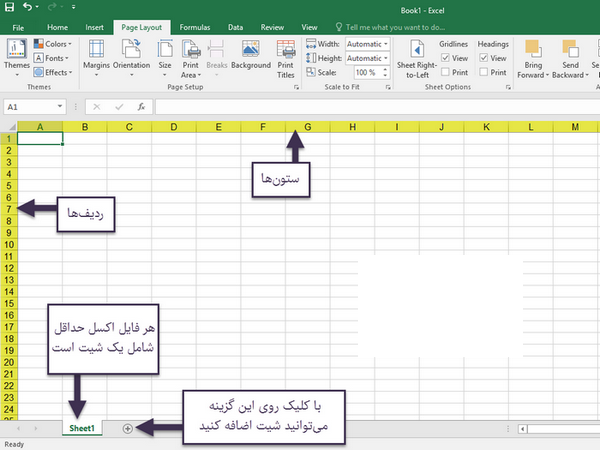
– Excel : از برنامه هاي معروف صفحه گسترده مي باشد كه براي كار با اعداد و ارقام، فرمولها، نمودارها و توابع كاربرد دارد. در اين برنامه تمامی محاسبههاي رياضي از جمع و تفريق گرفته تا واريانس و انحراف معيار قابل انجام است. ايجاد فرمول، مرتب سازی ستونها و سطرها، رسم انواع نمودارهاي ميلهاي، منحني، سلسله مراتبي، هرمي و… برخي از امكانات اين نرمافزار است.
– Powerpoint : برنامه اي ساده و جالب براي اسلايد سازي و نمايشهاي تبليغاتي می باشد. اين برنامه برای ايجاد فايلهاي Presentation طراحي شده است. ميتوان اسلايدهايي در رابطه با سخنراني يا مطلبی که قرار است جايي ارائه دهيم را تهيه كرده و از طريق ويدئو پروژكتور، آنها را روي پرده نمايش دهيم. ميتوان به اسلايدهاي خود حرکت و حالت هايي جالب اختصاص داد، انواع گرافيك و انيميشن را در آنها به كار برد و با اضافه كردن صداهاي گوناگون، آنها را جذابتر ساخت، صفحههاي مختلف را به هم پيوند داده و به راحتي بين اسلايدها حركت نمود.
– Access : از برنامه هاي بانك اطلاعاتي (پايگاه داده ها) محسوب شده و جهت سازماندهي اطلاعات مثل ليست تماس، كلكسيون موسيقي،ايجاد فرم هاي مخصوص درج اطلاعات و گزارش گيري كاربرد دارد. از طريق اين برنامه می توان به راحتي و در عرض چند دقيقه بانك اطلاعاتي دلخواه خود را ايجاد نمود. بانك اطلاعاتي، يك مجموعه از اطلاعات است. به عنوان مثال كليهي اطلاعات پرسنلي (از قبيل نام، نام خانوادگي، شماره شناسنامه…) معلمان و دانشآموزان يک مدرسه را می توان در يک بانک اطلاعاتی درون کامپيوتر نگهداري نمود.
برخي برنامه هاي ديگر اين مجموعه عبارتند از : Publisher، Outlook و …
قبول داريم که مجموعه حاضر عاری از کاستی ها و ايرادات نيست. اميدواريم با انتقادات و پيشنهادات خود در برطرف نمودن ايرادات و اشكالات اين اثر و ارسال پيام به نشانی tirotir2@gmail.com به ما ياري رسانيد.
مؤلفين
بخش نخست
توانايي کار با واژه پرداز Microsoft Word
1-1 آشنايی با تعريف واژه پرداز
– تايپ Typing : براي ايجاد يك سند، متن دلخواه را تايپ نموده و نتيجه كار را ذخيره(Save) مي سازيم.
– ويرايشEditing : عمليات تغيير، حذف، كپي، جابجايي را ويرايش گويند. (اين عمليات در ماشين تايپ ممكن نيست)
– قالب بنديFormatting : مي توان ظاهر مطالب تايپ شده را تغيير داد. مواردي از قبيل: فاصله ها، نوع قلم، اندازه و رنگ قلم، كار با جداول، كادرها.، سرصفحه و پاصفحه، چاپ، تصحيح خودكار غلط های املايي و گرامري و …
1-2 آشنايي با اجراي برنامه Word
از منوي Start گزينه All Programs و پس از آن Microsoft Office و نهايتاً Microsoft Office Word را كليك مي كنيم. با دابل كليك روي آيكنِ برنامه نيز مي توان آن را اجرا نمود.
1-3 آشنايی با محيط اصلي Microsoft Word
با توجه به شكل ، ابتدا با مهمترين قسمتهاي اين برنامه، بطور مختصر آشنا شده و سپس به جزييات بيشتري خواهيم پرداخت.
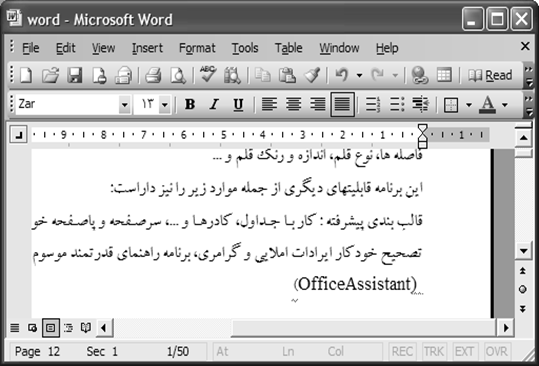
1-3-1 نوار عنوانTitle Bar
بالاترين نوار در محيط اين برنامه مي باشد. نام برنامه “Microsoft Word” و سپس نام پيش فرض براي سند باز شده فعلي”Document1” مشاهده مي گردد.
1-3-2 نوار منو Menu Bar
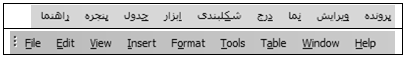
در زير نوار عنوان قرار داشته و ليستي از فرمانها را كه هر كدام از آنها نيز، يك ليست فرعي دارند، نمايش مي دهد. برخي از مهمترين اين فرمانها، براي راحتي كار، در نوار هاي ابزار برنامه قرار داده شده اند، كه بعداً به تفصيل شرح داده خواهند شد.
توسط اشاره گر ماوس و يا با فشردن كليد Alt و سپس كليدهاي جهت نما نيز قادريم گزينه دلخواه را در منو اجرا كنيم.
1-3-3 نوارهاي ابزارToolbars
برخي از مهمترين فرمانها بصورت آيكن در نوارهاي ابزار قرار داده شده است. معمولاً دو نوار ابزار زير در محيط برنامه بوده و وجود آنها بطور كلي لازم مي باشد.
1-3-3-1 نوار ابزار استاندارد
نوار ابزار استاندارد، در بالاي محيط اصلي برنامه Word قرار داشته و شامل فرمانهايي از قبيل ايجاد سند، باز نمودن سند، ذخيره، چاپ و … مي باشد.
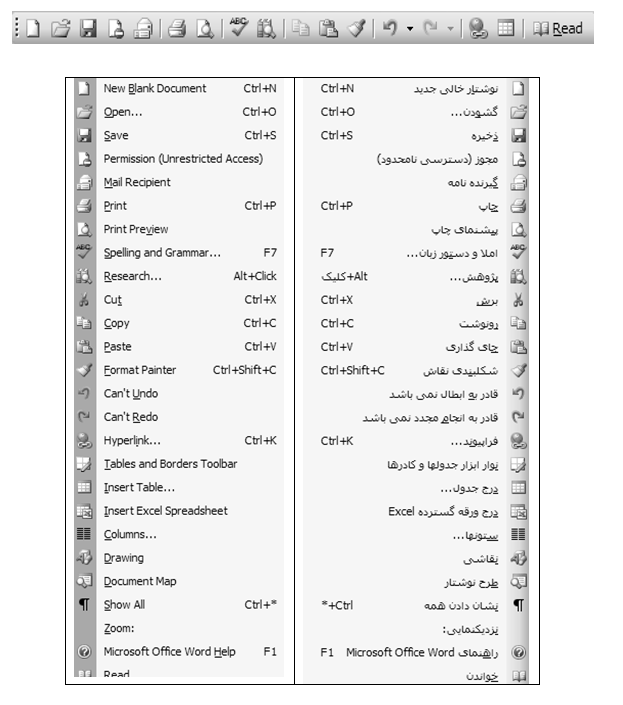
1-3-3-2 نوار ابزار Formatting
اين نوار ابزار شامل فرمانهاي بسيار مهمي مي باشد كه براي قالب بندي و فرم دهي به مطالبِ موجود در سندِ فعلي كاربرد دارند. قبلاً يادآور شده ايم كه بهتر است متن خود را ابتدا بطور كامل نوشته و ذخيره نموده و سپس آنرا قالب بندي و ويرايش نماييم. و البته مي توان قبل از شروع به نوشتن قالب خود را انتخاب و تنظيم نموده و سپس به تايپ بپردازيم.
اگر بعد از نوشتن، بخواهيم هر قسمتي از متن را قالب بندي و ويرايش نماييم، ابتدا بايد آن را انتخاب (بلوكه )نموده و سپس با استفاده از دكمه هاي نوار ابزار قالب بندي، تغييرات دلخواه را اعمال نماييم.
با راست كليك روي يكي از نوارهاي ابزار و يا از طريق گزينه Toolbars از منويView میتوان نوارهاي ابزار را پنهان و يا آشكار ساخت.
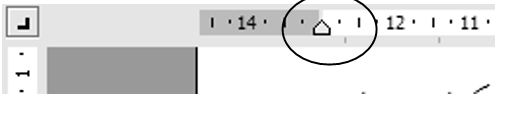
1-3-4 خط كشRuler
خط كش در زير نوارهاي ابزار و بالاي محيط تايپ مشاهده مي شود و براي تنظيم سريع متن سند كاربرد دارد. براي آشكار و يا مخفي ساختن خط كش مي توانيم از منوي View گزينه Ruler را انتخاب نماييم.
1-3-5 محيط تايپ (Text Area)
محيط بزرگ پايين خط كش را “Text Area” گويند.در اين منطقه به تايپ پرداخته و مطالب دلخواه را قرار مي دهيم. علامت چشمك زن گوشه بالا و راست يا چپ را مكان نما گويند. مطالب در محل فعلي مكان نما درج خواهند شد.در ضمن پس از ايجاد سند و تايپ متن دلخواه توسط گزينه Exit از منوي File برنامه Word خارج مي شويم. در صورتيكه نتيجه عمليات را ذخيره نكرده باشيم، پيام زير ظاهر خواهد شد:
“Do You Want To Save Changes To Document1?”
اگر Yesرا انتخاب نماييم، سند ذخيره شده ولي اگرNo را انتخاب نماييم، آنگاه سند بدون ذخيره شدن بسته خواهد شد!
1-3-6 نوار وضعيت (Status Bar)
اين نوار در پايين ترين قسمت محيط برنامه قرار دارد، و اطلاعات مهمي را درباره محل فعلي مكان نما، به نمايش مي گذارد.
در اين نوار ابزار با توجه به شكل بعد، اطلاعاتي درباره موارد زير داريم:
( Page ) شماره صفحه اي كه اكنون روي آن قرار داريم و فعال است.
( Sec) قسمت يا بخشي از سند كه مكان نما در روي آن قرار دارد.
( 1/1 ) دو عدد با علامت مميز / در بين آنها، نشان مي دهند ما اكنون در كدام صفحه (1 ) و مجموعاً كل سندمان چند صفحه است.
بقيه اعداد مثلا” At 1″ Ln.1 Col 1 نشان مي دهد اشاره گر ما اكنون در چه فاصله اي و چه سطر و ستوني قرار دارد.
| شماره صفحه فعلي |
| تعداد كل صفحات/شماره صفحه فعلي |
| شماره بخش |
| فاصله از بالاي صفحه |
| شماره ستون |
| شماره سطر فعلي |
1-3-7 نوارهاي پيمايش افقي(Horizontal) و عمودي(Vertical)
اين نوارها به ما امكان مي دهند تا سندي كه محتويات آن بيشتر از يك صفحه مي باشد را پيمايش نماييم. براي اين كار مي توان دكمه لغزنده موجود در نوار را به طرفين Drag نمود و يا اينكه روي دكمه هاي ابتدا و انتهاي نوار كليك مي كنيم.
مي توان نوار وضعيت، نوارهاي پيمايش افقي و عمودي را از منوي Toolsو گزينه Options و نهايتاً گزينه View آشكار ويا مخفي ساخت.
1-4 آشنايي با ايجاد سند جديد
روي نوار ابزار استاندارد دكمه را كليك نموده ويا گزينه New… را از منوي File انتخاب مي كنيم. ( با فشردن كليدهاي Ctrl + N نيز مي توان اين عمليات را انجام داد)
هر گاه گزينه New… را از منوي File برگزينيم،كادري باز مي شود كه مي توان توسط گزينه هاي آن كادر، يك سند نمونه با قالب بندي قبلاً تنظيم شده را انتخاب كرد، و سند فعلي خود را بر مبناي آن نمونه ايجاد نمود.
| ايجاديك سند جديد ايجاد يك سند جديد به كمك الگوها |
اگر از منوي View گزينه Task Pane علامت دار باشد، در آنصورت ليستي براي انجام وظايف،در سمت راست اين برنامه مشاهده خواهد شد. در حالت معمولی اگر گزينه Getting Started را در بالای ليست وظيفه (Task Pane)انتخاب کنيم، آنگاه يک ليست فرعی شامل برخی دستورات ظاهر خواهد شد.
1-5 آشنايي با چگونگی باز نمودن سند موجود
روي نوار ابزار استاندارد دكمه را كليك نموده ويا گزينه Open… را از منوي File انتخاب مي كنيم. (با فشردن كليدهاي Ctrl + O نيز مي توان اين عمليات را انجام داد)
1-6 آشنايي با ذخيره کردن سند فعلي با فرمتهای گوناگون
روي نوار ابزار استاندارد دكمه را كليك نموده ويا گزينه Save را از منوي File انتخاب مي كنيم(با فشردن كليدهاي Ctrl + S نيز مي توان اين عمليات را انجام داد). اگر بخواهيم از سند فعلي يك رونوشت با نامي متفاوت ويا در محلي ديگر تهيه نماييم، از منوي File گزينه Save As را انتخاب نموده و در كادر باز شده، تنظيمات لازم را انجام مي دهيم.
الف) در قسمت بالا (:Save In) محل ذخيره شدن را تعيين مي نماييم.
ب) در قسمت پايين (File Name) نامي را براي سند تايپ مي كنيم.
ج) در پايين ترين ليست بازشونده(Save As Type) نوع قالب بندي و پسوند سند را تعيين مي سازيم.
اگر قالب بندي سند را از .Doc به .Htm يا .Html تغيير دهيم آنگاه آن سند، براي قرار دادن در وب و اينترنت، مناسب خواهد بود.
1-7 آشنايی با اصول ويرايش متن
با استفاده از منوی Edit و بسياری از دکمه های نوار ابزار استاندارد وقالب بندی می توان عمليات ويرايشی مناسب را روی متن دلخواه اجرا نمود. در ادامه بدليل اهميت موضوع، مطالبی درباره تغيير زبان صفحه کليد، چگونگی انتخاب متن و عمليات کپی، بريدن، چسباندن، حذف متن و … را به تفصيل شرح خواهيم داد.
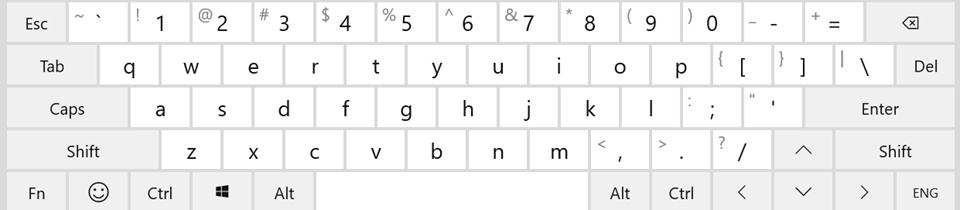
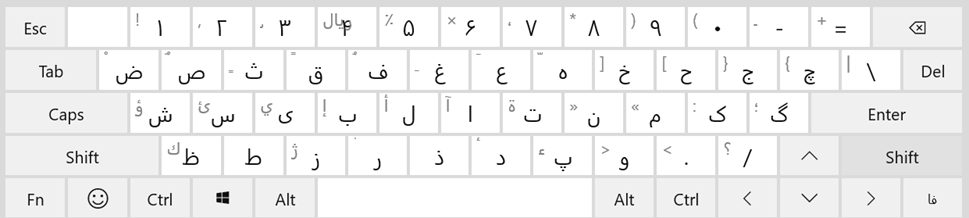
هر گاه ويندوز علاوه بر زبان انگليسي، قابليت فارسي نويسي و يا هر زبان ديگري داشته باشد، مي توان از طريق هاي مختلفي نوع زبانِ صفحه كليد را تغيير داد. مثلاً در نوار ابزار قالب بندي، دكمه چپ به راست(Left To Right) را كليك مي كنيم تا زبان صفحه كليد انگليسي شود. و يا دكمه راست به چپ (Right To Left) را براي فارسي شدن انتخاب مي كنيم.
همچنين مي دانيم كه در بسياري از مواقع، از دكمه هاي ) Ctrlيا (Altو Shift چپ براي انگليسي شدن و دكمه هاي Ctrl (يا Alt) و Shift راست براي فارسي شدن استفاده مي شود.
1-7-1 آشنايي با چگونگی انتخاب متن (Highlighting Text )
براي عمليات ويرايشي و قالب بندي مي بايست ابتدا متن موردنظر را به حالت انتخاب درآورد. به عنوان مثال اگر قصد داشته باشيم سطري از متنِ سند را در قسمتي ديگر از سند كپي نماييم، مي بايست قبل از هرچيز، آن سطر را به حالت انتخاب درآوريم. متن انتخاب شده برای قبول دستورات ويرايشی، رنگی و متمايز می شود.
چند روش براي انتخاب متن دلخواه از يك سند وجود دارد:
- مكان نما را در ابتدا يا انتهاي عبارت دلخواه قرار داده و كليد Shift را نگه مي داريم و سپس به كمك كليدهاي جهت نما به طرفين، حركت نموده و آن متن را به حالت انتخاب درمي آوريم.
- با دابل كليك روي كلمه موردنظر مي توان آن را به انتخاب درآورد.
- اشاره گر ماوس را به ابتدا يا انتهاي متن موردنظر انتقال داده و دكمه چپ را نگه داشته و ماوس را به سمت دلخواه حركت مي دهيم.
| متن انتخاب شده |
1-7-2 شناسايي اصول کپی، بريدن، چسباندن و حذف متن
گاهی لازم است قسمت زيادی از متن به جای ديگر از سند کپی، جابجا و يا حذف گردد. در اين هنگام می توان بدون دوباره کاری، از دستورات ساده ای به شرح زير استفاده نمود.
1-7-3 برش متن(Cut)
هر گاه قصد داشته باشيم متني را انتقال داده و جابجا نماييم، ابتدا آن متن را انتخاب كرده و سپس از نوار ابزار دكمه را انتخاب مي كنيم. يا اينكه روي آن متن راست كليك نموده و گزينه Cut را بر مي گزينيم. (با فشردن كليدهاي Ctrl + X نيز مي توان اين عمليات را انجام داد)
1-7-4 كپي متن (Copy)
هر گاه قصد داشته باشيم متني را كپي نماييم، ابتدا آن متن را انتخاب كرده و سپس از نوار ابزار دكمه را انتخاب مي كنيم. يا اينكه روي آن متن راست كليك نموده و گزينه Copy را بر مي گزينيم. (با فشردن كليدهاي Ctrl + C نيز مي توان اين عمليات را انجام داد)
1-7-5 چسباندن متن(Paste)
هنگامي كه موضوعي را Copy يا Cut كنيم آن موضوع در حافظه موقت قرار می گيرد، مي توان يک نسخه از آن موضوع را در محل موردنظر قرارداد.
اگر بخواهيم متن Cut يا Copy شده را در قسمتي از سند بچسبانيم، ابتدا مكان نما را به محل موردنظر(مقصد) مي بريم و سپس از نوار ابزار دكمه را انتخاب مي كنيم. يا اينكه در آن محل، راست كليك نموده و گزينه Paste را بر مي گزينيم(با فشردن كليدهاي Ctrl + V نيز مي توان اين عمليات را انجام داد). البته مي توان مطلب Cut يا Copy شده را در اسناد ديگر و حتي در اسناد برخي برنامه هاي مرتبطِ ديگر، قرار داد.
در ضمن عمليات Copy و Cut را از منوی Edit نيز می توان انجام داد.
1-7-6 حذف متن
ابتدا متن موردنظر را انتخاب نموده و سپس دکمه Delete را روی صفحه کليد فشار می دهيم و يا اين که از منوی Edit گزينه Clear را انتخاب نموده و يکی از دستورات موجود در منوی فرعی را اجرا می کنيم:
- Formats : فقط قالب بندی متن انتخاب شده حذف می گردد.
- Contents : کل متن انتخاب شده حذف خواهد شد.
1-7-7 رنگ زمينه قلم (Highlight)
براي انتخاب و Highlight كردن متن و تنظيم رنگي براي زمينه آن، دكمه در نوار ابزار قالب بندي كاربرد دارد.
1-7-8 رنگ قلم (Font Color)
دكمه در انتهاي سمت راست نوار ابزار قالب بندي براي تغيير رنگ قلم مي باشد.
1-7-9 آشنايي با استفاده از دستور برگشت
هر گاه درعمليات تايپ، ويرايش و قالب بندي كاري انجام داده و بخواهيم آن كار ناديده گرفته شده و متن به حالت قبل برگردد، دكمه لغو عمليات قبلي(Undo ) را در نوار ابزار استاندارد انتخاب مي كنيم (با فشردن كليدهاي Ctrl + Z نيز مي توان اين عمليات را انجام داد).
در ضمن برای ناديده گرفتن و لغو عمليات Undo دكمه انصراف از لغو ( Redo) را در نوار ابزار كليك مي كنيم.
1-7-10 آشنايي با نحوه ضخيم و پررنگ کردن متن انتخاب شده Bold))
دكمه در نوار ابزار قالب بندي، متن انتخاب شده را ضخيم و پررنگ مي سازد. (Ctrl + B)
1-7-11 آشنايي با نحوه زير خط دار کردن متن انتخاب شده (Underline)
دكمه در نوار ابزار قالب بندي براي زير خط دار كردن متن انتخابي مي باشد. (CTRL+U)
1-7-12 آشنايي با نحوه مايل و ايتاليك کردن متن انتخاب شده (Italic)
دكمه در نوار ابزار قالب بندي براي مايل كردن متن انتخابي مي باشد. (CTRL+I)
به عنوان مثال با توجه به مطالب فوق، سطرهايي را تايپ نموده و به حالتهاي معمولي،ضخيم، زيرخط دار و مايل در مي آوريم:
| اين سطر در حالت معمولي است. اين سطر در حالت ضخيم است. اين سطر در حالت زير خط دار است. اين سطر در حالت مايل است. |
1-7-13 آشنايي با ابزار چيدمان
برای تنظيم و مرتب نمودن متن در نوار ابزار قالب بندي تنظيمات زير امکان پذير مي باشد.
| چپ چين شدن متن | Align Left | |
| وسط چين شدن متن | Center | |
| راست چين شدن متن | Align Right | |
| همتراز از دو طرف | Justify |
هرگاه در جايي از يك سطر يا پاراگراف كليك نموده و يكي از دكمه هاي فوق را فشار دهيم، متن آن قسمت، نسبت به لبه كاغذ، مرتب و تراز خواهد شد.
مثال) در متن زير سطر اول وسط چين، سطر دوم راست چين و سطر سوم چپ چين مي باشد.
به نام خدا
توانا بود هركه دانا بود
ز دانش دل پير برنا بود
1-8 شناسايي اصول تنظيم قلم و اندازه قلم
براي تغيير سبك، نوع و اندازه قلم ابتدا متن موردنظر را انتخاب نموده و سپس توسط دكمه اول اين نوار ابزار(Style) سبك قلم را تغيير داده و توسط دكمه دوم(Font) نوع قلم را تغيير مي دهيم و به كمك دكمه سوم (Font Size) اندازه قلم را تنظيم مي سازيم.
| انتخاب يك سبك و حالت براي قلم |
| نوع قلم |
| اندازه قلم |
| تغيير زبان |
به عنوان مثال سطري را تايپ نموده و به حالت انتخاب درآورده و سپس توسط دكمه هاي نوار ابزار قالب بندي(مطابق شكل قبل) ويرايش لازم را انجام مي دهيم
1-8-1 سربرگ Font از کادر Format
همچنين از طريق منوي Format و گزينه Font… نيز مي توان ظاهر قلم را تغيير داد. به شكل بعد و توضيحات آن توجه فرماييد.
اگر پس از تنظيمات دلخواه، دكمه را در پايين و چپ انتخاب كنيم، آنگاه تنظيمات انجام شده هميشگي و دايمي خواهند شد.
توجه شود كه در قسمت مياني كادر فوق(Effects)، مي توان با انتخاب گزينه هاي زير، اعداد و يا متن انتخاب شده فعلي را بالا نويس (حالت توان) و يا پايين نويس(حالت انديس) نمود.
Superscript : بالا نويس (حالت توان) مثل اعداد2 و 5 در عبارت 32+45 = ?
(البته از كليدهاي تركيبي Ctrl+Shift+(+) نيز ميتوان استفاده نمود.)
Subscript: پايين نويس(حالت انديس) مثل اعداد 2 و 10 در عبارت (110101)2 = (?)10
(البته از كليدهاي تركيبي Ctrl+(+) نيز ميتوان استفاده نمود.)
1-8-2 برگه Character Spacing (برگه دوم از كادر Font)
در صفحه محاوره اي اين برگه، توسط قسمت Scale ميتوان كاراكترهاي قلم را فشرده ساخت يا باز نمود. قسمت Spacing در اين برگه، فاصله بين حروف يك كلمه را تغيير داده وكم و يا زياد مي كند. و قسمت Position براي جابجايي متن سند نسبت به خط اصلي مي باشد. (Lowered) پائين تر و (Raised) بالاتر از خط اصلي .
1-8-3 برگه Text Effects (برگه سوم از كادر Font)
اگر متن خود را بلوك كرده و يكي از گزينه هاي اين كادر محاوره اي را انتخاب كنيم آنگاه دور متن انتخابي ما جلوه هاي متحرك و جالبي نمايان ميشود. البته اين Animation و جلوه ها ارزش چاپي ندارند.
1-9 آشنايي با چگونگی استفاده از پيوند در مکان مناسب(Hyperlink)
اگر بخواهيم متني شبيه صفحات وب بوده و داراي پيوند باشد، و با كليك در آن متن صفحه و برنامه جديدي ظاهر گردد، از دكمه استفاده مي كنيم.
1-10 آشنايي با حالتهای مختلف نمايش سندDocument View
در اين برنامه مي توان از منوي View يكي از حالات نمايشي زير را تنظيم نمود:
Normal, Web Layout, Print Layout, Reading Layout, Outline
در اين قسمت بطور مختصر هر كدام از حالات نمايشي فوق شرح داده مي شود:
– Normal : در اين نما قالب بندی متنِ سند در حالت معمولي نمايش داده خواهد شد.
– Web Layout : نمايش سند بصورتي كه در برنامه مرورگر وب مشاهده خواهد شد.
– Print Layout : در اين حالت سند به همان شكلي كه قرار است چاپ شود، نمايش داده خواهد شد.
–Reading Layout : اين حالت برای مطالعه سند مناسب است.
– Outline : در اين حالت طرح کلی سند شامل عناوين اصلی و فرعی نمايش داده خواهد شد.
در ضمن در گوشه پايين و چپِ محيط برنامه Microsoft Word دكمه هايي براي تغيير وضعيت نمايشي در دسترس است(با عملكردي مشابه با گزينه هاي مشروح فوق)
1-11 آشنايي با ابزارهای بزرگ نمايي و کوچک نمايي سند(Zoom)
در انتهاي سمت راست نوار ابزار استاندارد، ليست باز شونده اي در دسترس است ( ) كه از طريق آن مي توان بزرگ نمايي سند را تغيير داد. مثلاً هر گاه اين گزينه، روي %200 تنظيم باشد، سند دوبرابر بزرگتر مشاهده خواهد شد. راه ديگر اين است كه مي توان از منوي File گزينه Zoom را انتخاب نمود و در كادر كوچك بازشده، درصد بزرگنمايي را مشخص ساخت.
1-12 آشنايي با چگونگی تايپ يک پاراگراف جديد
از نظر برنامه Microsoft Word هر گاه كليد Enter فشرده شود،پاراگراف فعلي خاتمه پذيرفته و پاراگراف جديدي آغاز خواهد شد. پاراگراف می تواند يک حرف، يک کلمه يا چندين سطر باشد.
از منوي Format گزينه Paragraph كادر پاراگراف را نمايان خواهد ساخت كه در آن مي توان تنظيماتي از قبيل فاصله بين پاراگرافها را انجام داد.
براي نمايش اطلاعاتي از قبيل تعداد پاراگرافها و فاصله ها در سند، مي توان دكمه را در نوار ابزار استاندارد کليک نمود.

1-13 فرو رفتگی و بيرون رفتگی ابتدای يك پاراگراف
دكمه در نوار ابزار قالب بندی جهت تو رفتگي يك پاراگراف كاربرد دارد. برای بيرون رفتگی پاراگراف، در سطر دلخواهي كه نسبت به حاشيه چپ يا راست تو رفته است كليك نموده وسپس دكمه را در نوار ابزار قالب بندي انتخاب مي كنيم تا فاصله آن متن نسبت به حاشيه تغيير نمايد. اگر فاصله متن نسبت به حاشيه كاغذ زياد شود، آن متن تورفتگي يافته و اگر فاصله آن كم شود، آن متن بيرون رفتگي يافته است.
| ميزان تو رفتگي قبول داريم که مجموعه حاضر عاری از کاستی ها و ايرادات نيست، اما می تواند قدم مثبتی در جهت ارتقا دانش فني علاقمندان تلقي شود. انشاءا… مفيد واقع گردد. |
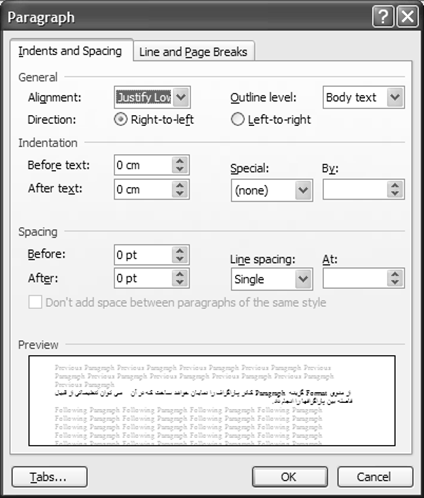
1-14 آشنايي با تغيير فاصله بين سطرها Line Spacing) )
اين فرمان ميزان فضاي بين سطرهاي يك پاراگراف را تنظيم مي كند. در قسمت پايين كادر Paragraph از منوي Format مي توان فاصله بين سطرها را تنظيم نمود. به عنوان نمونه، اگر Double را انتخاب كنيم فاصله بين سطرهاي انتخاب شده فعلي، دو برابر خواهد شد و اگر 1.5 Lines را برگزينيم، فاصله بين سطرها يك و نيم برابر خواهد شد.
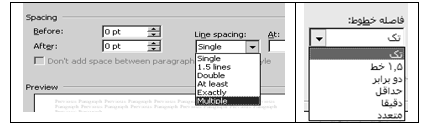
در ادامه همين بحث، يك پاراگراف را با فاصله هاي متفاوتِ بين سطرها،با ذكر كليدهاي تركيبي مربوطه نشان داده ايم:
| الف)براي اينكه فاصله بين سطرها در حالت معمولي باشد، پس از انتخاب سطرها، كليدهايCtrl + 1 را روی صفحه كليد مي زنيم: |
| هرگز هيچ هدفي را رها مكنيد، مگر اينكه ابتدا قدم مثبتي در جهت تحقق آن برداشته باشيد. هم اكنون لحظه اي فكر كنيد و اولين قدمي را كه بايد در جهت رسيدن به هدف برداريد مشخص سازيد. براي اينكه پيشرفت كنيد، چه قدمي را بايد امروز برداريد؟ حتي يك قدم كوچك شما را به هدف نزديكتر مي كند. |
| ب) براي اينكه فاصله بين سطرها 1.5 برابر باشد، پس از انتخاب سطرها، كليدهايCtrl + 5 را روی صفحه كليد مي زنيم: |
| هرگز هيچ هدفي را رها مكنيد، مگر اينكه ابتدا قدم مثبتي در جهت تحقق آن برداشته باشيد. هم اكنون لحظه اي فكر كنيد و اولين قدمي را كه بايد در جهت رسيدن به هدف برداريد مشخص سازيد. براي اينكه پيشرفت كنيد، چه قدمي را بايد امروز برداريد؟ حتي يك قدم كوچك شما را به هدف نزديكتر مي كند. |
| ج) براي اينكه فاصله بين سطرها 2 برابر باشد، پس از انتخاب سطرها، كليدهايCtrl + 2 را روی صفحه كليد مي زنيم: |
| هرگز هيچ هدفي را رها مكنيد، مگر اينكه ابتدا قدم مثبتي در جهت تحقق آن برداشته باشيد. هم اكنون لحظه اي فكر كنيد و اولين قدمي را كه بايد در جهت رسيدن به هدف برداريد مشخص سازيد. براي اينكه پيشرفت كنيد، چه قدمي را بايد امروز برداريد؟ حتي يك قدم كوچك شما را به هدف نزديكتر مي كند. |
1-15 آشنايي با درج صفحه گسترده در سند
دكمه (Insert Microsoft Excel Worksheet) را در نوار ابزار انتخاب مي كنيم تا يك صفحه گسترده از برنامه اكسل در محل مكان نما ايجاد شود.
1-16 شناسايي اصول ايجاد جدول و عمليات بر روی آن
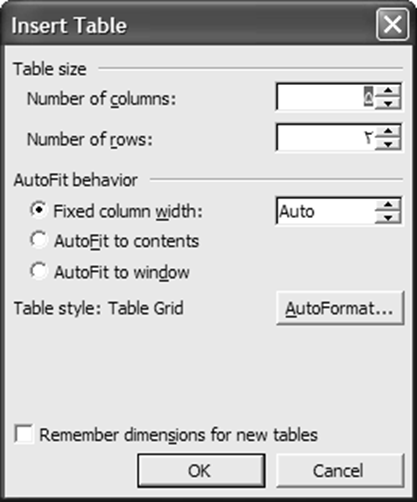
براي رسم سريع جدول از دكمه Insert Table استفاده مي گردد. هر گاه اين دكمه نگه داشته شود، در آن صورت كادر كوچكي ظاهر مي شود و ما در اين كادر، تعداد سطرها و ستونهاي جدول را مشخص مي سازيم.

رسم جدولي با سه سطر و دو ستون
در ضمن مي توان از منوي Table ، براحتي از طريق گزينه Insert جدول دلخواه را ساخت، تغيير داد و مديريت نمود. به شكل بعد توجه نماييد كه 2 سطر و 5 ستون تعيين شده است.
| تعداد ستون تعداد سطر قالب بندي خودكار جدول |
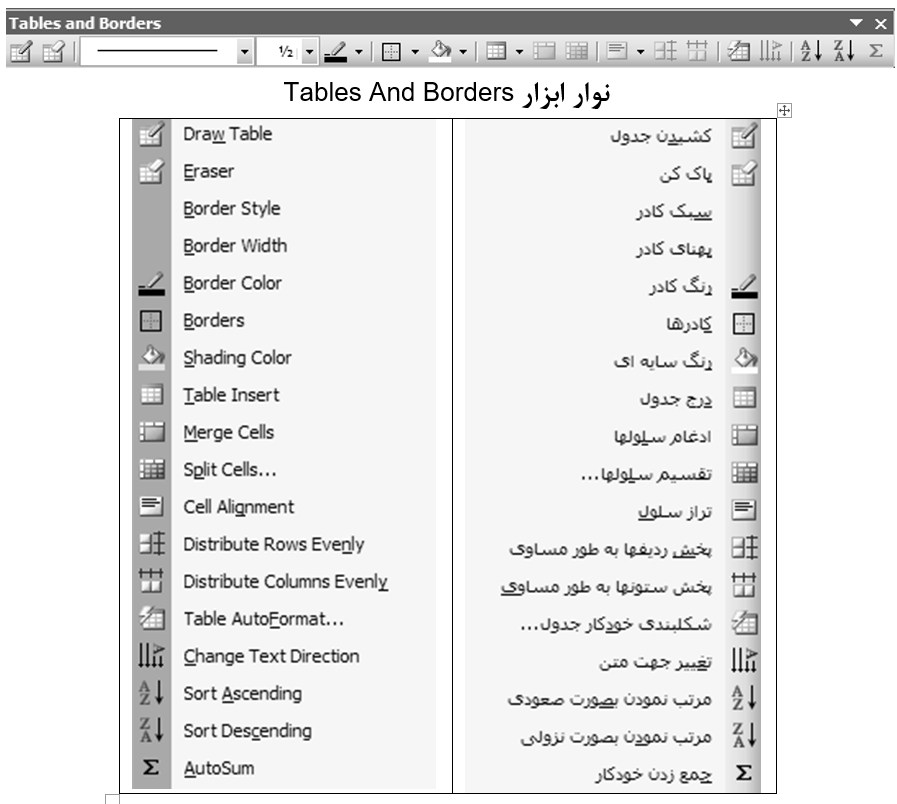
1-16-1 نمايش نوار ابزار جدولها و كادرها
براي رسم جدول و تغييرات در آن، مي توانيم دكمه را انتخاب نموده و توسط دكمه هاي اين نوار، تنظيمات دلخواه را انجام دهيم.
1-16-2 تقسيم يک خانه از جدول به چند خانه
با راست كليك در يك خانه از جدول و انتخاب گزينه Split… مي توان آن خانه را به چند خانه (در چند سطر و ستون) تجزيه و تقسيم نمود.كادري مشابه شكل بعد ظاهر شده و ما قادر خواهيم بود كه تنظيم نماييم خانه مذكور به چند سطر (Row) و چند ستون (Column) تجزيه شود.
پس از آن كه با استفاده از منوي Table يك جدول با تعداد سطر و ستون دلخواه (مثلاً 2 سطر و 5 ستون) ايجاد نموديم، آنگاه خانه اي از جدول را كه مي خواهيم به چند خانه تجزيه كنيم را انتخاب نموده و سپس روي اين خانه انتخاب شده، راست كليك نموده و گزينه Split را کليک می کنيم تا كادر شكل بعد نمايان شود. در اين كادر تنظيم مي كنيم كه خانه انتخاب شده به چند ستون و سطر تجزيه شود.
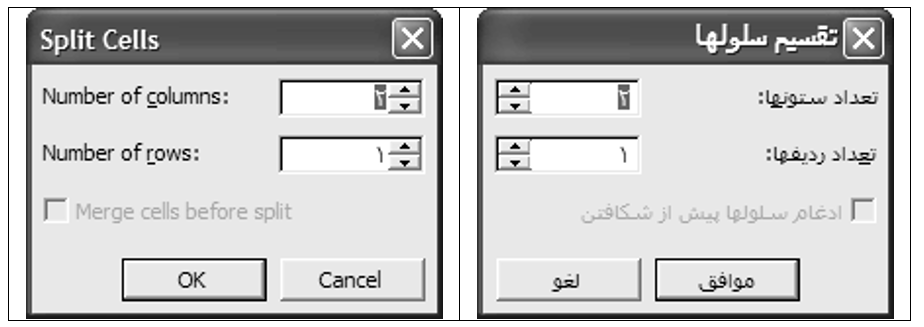
( در اين كادر تنظيم شده كه خانه انتخاب شده به 2 ستون و 1 سطر تجزيه گردد)
| اين خانه ابتدا انتخاب شده و سپس به 2 ستون و يک سطر تجزيه(Split) شده است. |
1-16-3 ادغام چند خانه از جدول در يک خانه
براي ادغام و يكي نمودن چند خانه در يك خانه، ابتدا آن خانه ها را انتخاب نموده و سپس روي يكي از خانه هاي انتخاب شده، راست كليك نموده و گزينه Merge… را بر مي گزينيم.
| جدولي با 4 ستون و 3 سطر انتخاب خانه هاي دلخواه ادغام خانه هاي انتخاب شده |
اين خانه ها ابتدا انتخاب شده و سپس ادغام(Merge) شده اند.
þبراي ادغام و حذف خانه هايي از جدول،مي توان از نوار ابزار Borders & Tables پاك كن (Eraser) را انتخاب نمود و سپس روی خطی که وسط دو خانه قرار گرفته کليک كرد تا آن خط حذف شود.در ارتباط با عمليات ادغام و حذف راه ديگر اين که از منوی Table گزينه Splite يا Merge را انتخاب کنيم.
1-16-4 تغيير اندازه جدولها
براي اينكه بتوانيم عرض و يا ارتفاع خانه هاي جدول خود را كم و زياد كنيم ، كافيست تا اشاره گر را بين دو خانه قرار داده و هنگامي كه اشاره گر به شكل يك فلش دو طرفه شود با كشيدن خط به يك سمت ديگر،تغييرات موردنظر را انجام دهيم.
1-16-5 تايپ عمودی در خانه های جدول
براي تايپ عمودي در جدول ابتدا خانه مورد نظر را انتخاب نموده سپس از منوي Format، گزينه Text Direction را انتخاب مي سازيم.
1-16-6 قالب بندی خودکار
اگر از منوي Table گزينه Table Auto Format (قالب بندي خودكار) را انتخاب كنيم خواهيم توانست از طرح هاي آماده برنامه Wordبراي ايجاد جدول استفاده كنيم.
1-16-7 اضافه کردن ستون و سطر جديد
جهت اضافه كردن يك ستون می توان از منوي Table گزينه Insert و سپس Colmuns… را انتخاب نمود . و براي اضافه كردن يك سطر يا رديف می توان از منوي Table گزينه Insert و سپس Rows… را انتخاب كرد. و براي اضافه كردن خانه می توان از منوي Table گزينه Insert و سپس Cells… را انتخاب نمود .
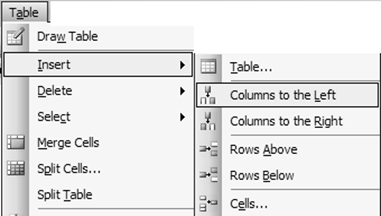
1-16-8 حذف ستون يا سطر
براي حذف يك ستون ، يك رديف يا يك خانه می توان از منوي Table گزينه Delete را بكار برد.
1-17 آشنايي با چگونگی کار دکمه های نوار ابزار ترسيمات (Drawing)
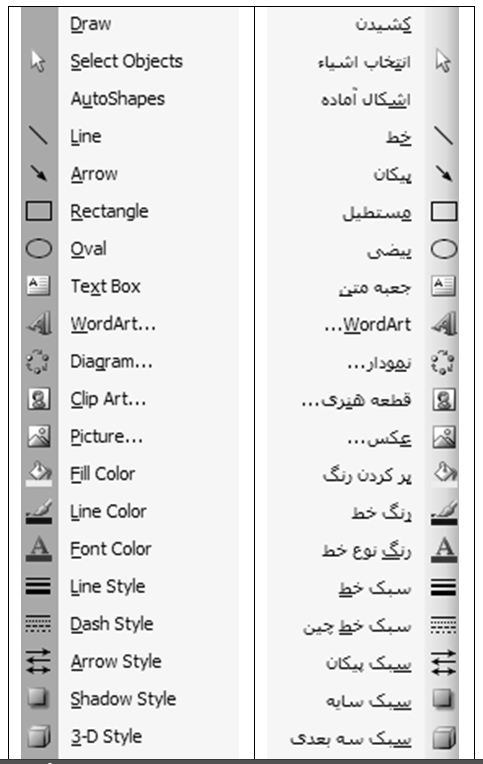
دكمه براي نمايان ساختن نوار ابزار ترسيمات كاربرد دارد. توضيحات مربوط به اين نوار در ادامه شرح داده شده است.
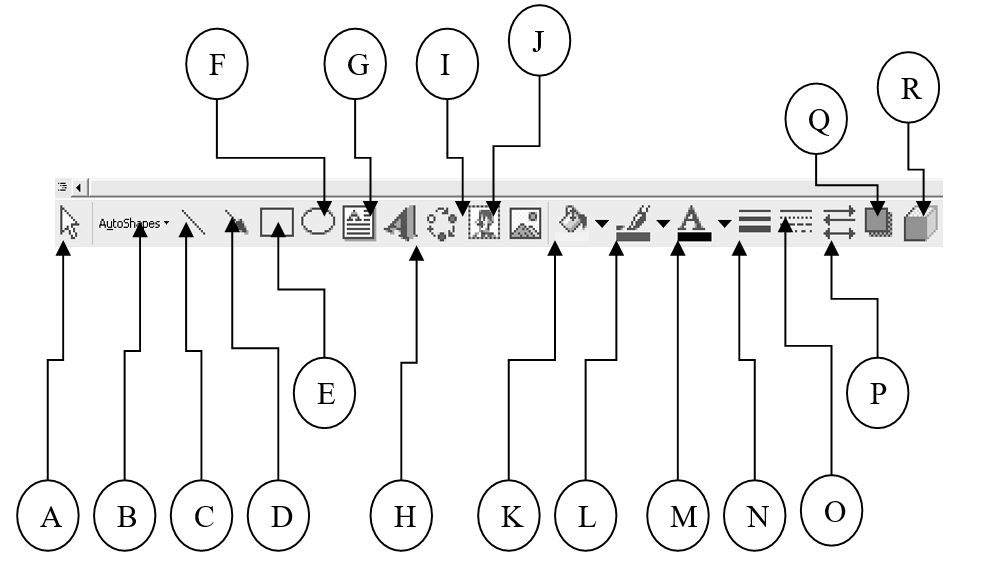
- برای رسم برخي اشكال هندسي آماده(Autoshapes) به کار می رود.
B– برای رسم خط(Line) استفاده می شود.
C– برای رسم پيكان(فلش) (Arrow) کاربرد دارد.
D– برای رسم مستطيل (Rectangle) کاربرد دارد.
E– برای رسم بيضي (Oval) به کار می رود.
F– برای رسم جعبه متني (Text Box) استفاده می شود.
G– برای رسم كلمات هنري با جلوه هاي ويژه (Wordart) استفاده می شود.
H– برای رسم نمودار استفاده می شود.
I– برای درج اشكال گرافيكي آماده استفاده می شود.
J– برای درج تصوير (Insert Picture) استفاده می شود.
K– برای رنگ كردن داخل اشكال هندسي انتخابی (Fill Color) استفاده می شود.
L– برای رنگ كردن خطوط اشكال هندسي انتخابی (Line Color) استفاده می گردد.
M– برای رنگ قلم (Font Color) استفاده می شود.
N– برای تغيير ضخامت خطوط اشكال هندسي انتخابی (Line Style) استفاده می شود.
O– برای تغيير نوع و حالت خط اشكال هندسي انتخابی (Dash Style) استفاده می شود.
P– برای تغيير حالت پيكان(فلش) (Arrow Style) استفاده می شود.
Q– برای سايه دار كردن اشكال (Shadow Style) استفاده می شود.
R– برای سه بعدي نمودن اشكال (3-D Style) استفاده می شود.
1-18 آشنايي با چگونگی استفاده از برنامه راهنما (Help)
با انتخاب گزينه از منوی Help و يا با فشردن دكمه در نوار ابزار استاندارد كادري باز مي شود كه بايد در آن سوال خود را مطرح نمود،تا برنامه درباره آن سوال توضيحاتي را در صورت وجود نمايش دهد. بنابراين عبارتي را در آن تايپ نموده و Enter را انتخاب مي كنيم. كه در صورت وجود آن عبارت در كتابچه راهنماي برنامه، ليستي ظاهر شده و سرفصل مربوط به آن عبارت را ظاهر مي سازد، كه با كليك روي يكي از موارد موجود در ليست، مطلب مربوط به آن عبارت نمايان مي شود. در صورت نياز مي توانيم آن مطلب را Copy نموده و در سند Paste نماييم.
به عنوان مثال درباره Table اطلاعاتي را جستجو مي کنيم:
پس از تايپ اين کلمه در قسمت تعيين شده، کليد Enter را فشار داده و يا دکمه را در مقابل اين قسمت انتخاب می سازيم. تا در کتابچه راهنما، ليستی از عنوان های مربوط به Table نمايان شود.
هر گاه يکی از اين عنوان ها را انتخاب سازيم، توضيحات و مطلب مرتبط با آن عنوان مشاهده خواهد شد.
1-19 آشنايي با چگونگی استفاده از ابزار بررسی کننده املايي و دستوری
براي تصحيح خودكار ايرادات املايي و دستوري مي توان روي نوار ابزار استاندارد دكمه را كليك نموده ويا گزينه Spelling And Grammar را از منوي Tools انتخاب كرد (با فشردن كليد F7 نيز مي توان اين عمليات را انجام داد).
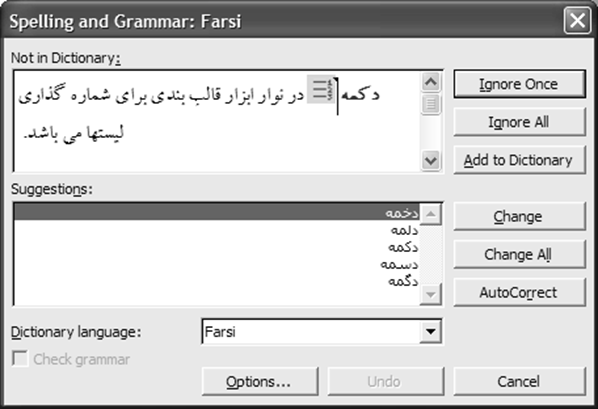
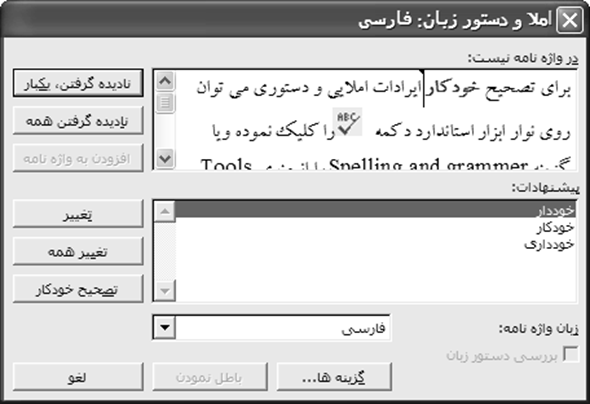
مي توان در اين برنامه از طريق دكمه Options… در پايين، كادر تنظيمات مربوط به Spelling and Grammar را ظاهر ساخته و گزينه ها ي دلخواه را غير فعال ساخته و در صورت نياز مجدداً آنها را فعال نمود.
در شكل بعد گزينه هاي Spelling and Grammar را با توضيح فارسي ملاحظه نماييد.
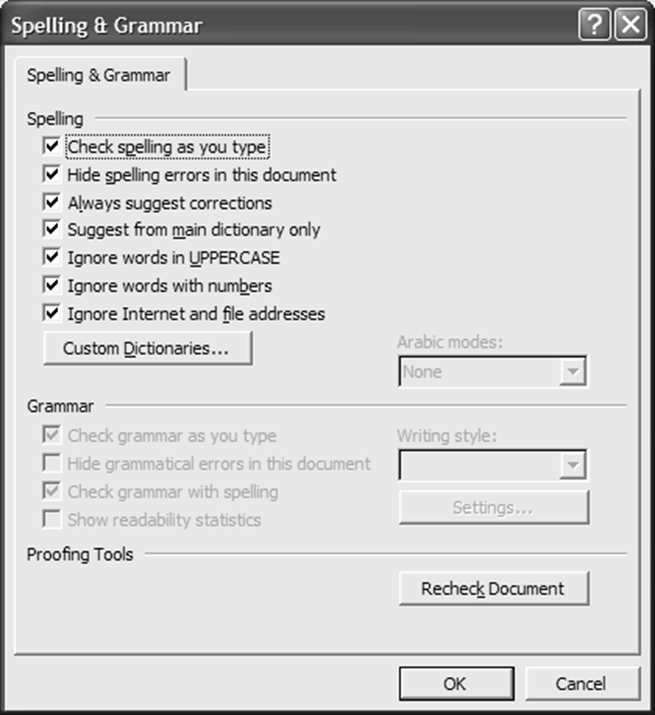
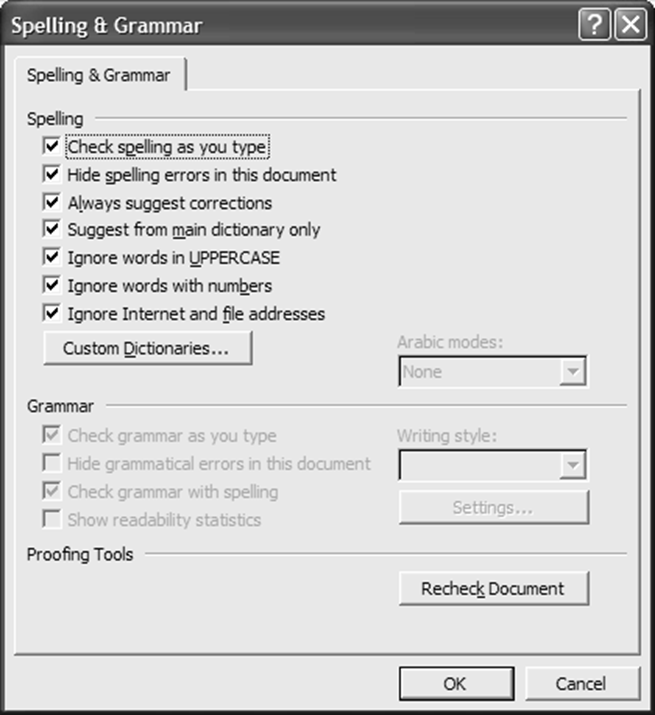
اين برنامه يك ديكشنري هوشيار دارد كه در هنگام تايپ، طبق اين فرهنگ لغت املاي مطالب تايپ شده را چك نموده و اگر غلط ديكته داشته باشد زير آن كلمه خط قرمز و اگر غلط گرامري وجود داشته باشد خط سبز رنگ مي كشد. از طريق دکمه اين امکان وجود دارد که فرهنگ لغت ديگری را تعيين نمود و يا اين که از اين عمليات صرف نظر کرد.
1-20 آشنايي با استفاده از فهرستهای اعداد و علامتها
دكمه در نوار ابزار قالب بندي براي شماره گذاري ليستها (Numbering) مي باشد. در ضمن از منوي Format گزينه Bullets And Numbering… كادر مربوط را جهت تغيير نوع شماره گذاري و تنظيمات بيشتر نمايان خواهد ساخت. در برگه Numbered يكي از حالتها را انتخاب نموده و كادر را تاييد مي كنيم.
برای نمونه به چند نوع شماره گذاري زيرتوجه می کنيم:
| پوريا سينا پدرام | پورياسيناپدرام |
| پورياسيناپدرام | پورياسيناپدرام |
دكمه در نوار ابزار قالب بندي براي علامت گذاري ليستها (Bullets) مي باشد. در ضمن از منوي Format گزينه Bullets And Numbering… كادر مربوط را جهت تغيير نوع شماره گذاري و تنظيمات بيشتر نمايان خواهد ساخت. در برگه Bulleted يكي از حالتها را انتخاب نموده و كادر را تاييد مي كنيم.
به عنوان مثال به چند نوع علامت گذاري زير توجه می کنيم:
| پورياسيناپدرام | پورياسيناپدرام |
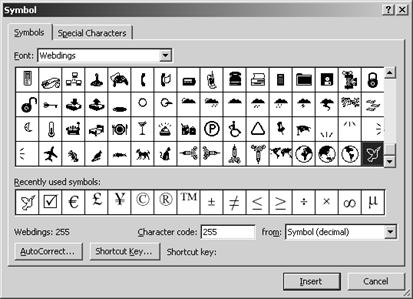
نكته) براي اينكه علامتهاي جالب و سفارشي بسازيم، بايد مراحل زير را انجام دهيم:
در برگه Bulleted از كادر Bullets And Numbering… يك علامت را انتخاب مي كنيم تا طي مراحلي، علامت ديگري را جايگزين آن سازيم.
- دكمه را در پايين و راست اين برگه انتخاب مي كنيم.
دكمه Character را براي انتخاب نوع علامت كليك مي كنيم. از ليست باز شونده بالاي كادر بعد، نوعي قلم(مثلاً Webdings ) را انتخاب مي نماييم:
دکمه Font امکان تنظيم قالب بندی قلم(نوع، اندازه، رنگ و …) را در اختيار قرار می دهد.
5) در ميان علائم نمايان شده، شكل و علامت دلخواه را انتخاب نموده و كادرها را بترتيب تاييد مي كنيم.
| مثال) غزال تارا شادي نگار ساينا |
1-21 آشنايي با چگونگی ايجاد صفحات جديد در سند فعلی
هر گاه مطالب تايپ شده از اندازه صفحه تجاوز نمايد، اين برنامه بطور هوشمند صفحه جديدی ايجاد می کند. اما بطور کلی براي ايجاد صفحه جديد در سند فعلی، ابتدا مكان نما را به جايي از صفحه كه مي خواهيم، صفحه جديدي از آن نقطه به بعد ايجاد شود منتقل نموده و از منوي Insert گزينه Break را انتخاب و Ok را كليك مي نماييم و يا اينكه از كليدهاي تركيبيِ Ctrl و Enter استفاده مي كنيم.
1-22 آشنايي با اضافه کردن سرصفحه و پاورقی (Header And Footer)
هرگاه از منوي View گزينه Header And Footer را انتخاب نماييم، كادر نقطه چيني در بالاي صفحه و همچنين نوار ابزاري خاص نمايان مي شود كه در كادر نقطه چيني مطلب دلخواه را به عنوان سرصفحه تايپ مي كنيم.
دكمه هاي اين نوار ابزار در تنظيم سرصفحه و پاصفحه كاربرد دارند.
A – برای درج يك متن و عبارت آماده استفاده می شود.
B– برای شماره بندي صفحات استفاده می شود.
C – برای درج تعداد كل صفحات سند فعلي استفاده می شود.
D – برای تغيير قالب شماره بندي صفحات استفاده می شود.
E – برای درج تاريخ فعلي سيستم استفاده می شود.
F – برای درج ساعت فعلي سيستم استفاده می شود.
G – برای دسترسی به كادر تنظيمات صفحه استفاده می شود.
H – برای مخفي کردن متن سند در زمان تنظيم سرصفحه و پاصفحه استفاده می شود.
I – برای اعمال تنظيمات مشابه صفحه قبل سند در صفحه جاری استفاده می شود.
J – برای انتقال مكان نما بين سرصفحه و پاصفحه جهت تنظيم هركدام استفاده می شود.
K– برای جابجايي بين صفحات زوج و فرد (صفحات قبل و بعد) استفاده می شود.
L– برای بستن نوار ابزار فوق و برگشت به محيط معمولي برنامه استفاده می شود.
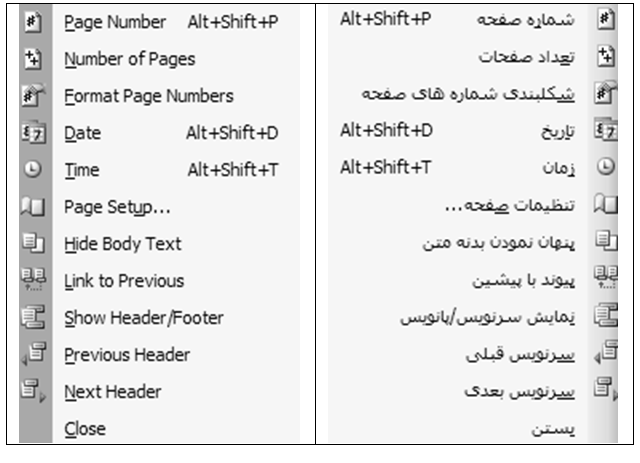
1-23 آشنايي با شماره بندي صفحات سند
از منوي Insert گزينه Page Numbers را انتخاب نموده ودر كادر باز شده از ليست بازشونده بالايي تعيين مي كنيم كه شماره صفحات بالا يا پايين باشند. از ليست بازشونده پاييني تعيين مي نماييم كه شماره صفحات چپ يا راست باشند.
| تنظيم اينكه صفحه اول نيز، شماره صفحه داشته باشد. |
اگر دكمه …Format در كادر فوق را فشار دهيم، كادري باز خواهد شد كه در آن قادريم نوع شماره را تغيير دهيم و همچنين تنظيم نماييم كه عمليات شماره بندي اين سند، از چه شماره اي آغاز شود.
| تعيين اينكه شماره گذاري سند فعلي، از عدد خاصي شروع شود. |
1-24 آشنايي با قرار دادن كاراكترهاي ويژه در سند
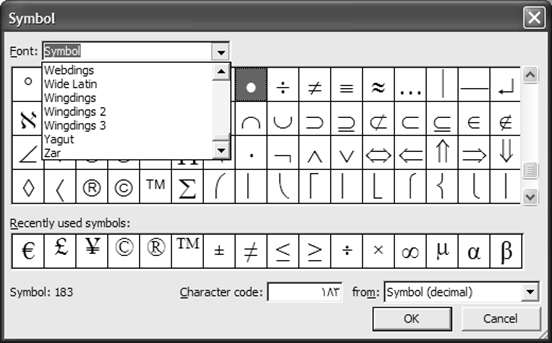
از منوي Insert گزينه Symbol را انتخاب نموده و از ليست باز شونده بالاي كادر باز شده، نوعي قلم را انتخاب نموده و از جدول كاراكترها، يكي را كليك نموده و سپس دكمه Insert را در پايين كادر مي زنيم تا كاراكتر انتخاب شده در محل فعلي مكان نما درج گردد.
1-25 آشنايي با درج تصوير، نمودار و اشياء ديگر
برای درج تصاوير مختلف از منوي Insert گزينه Picture و پس از آن با توجه به شکل بعد يکی از گزينه ها را انتخاب می سازيم.
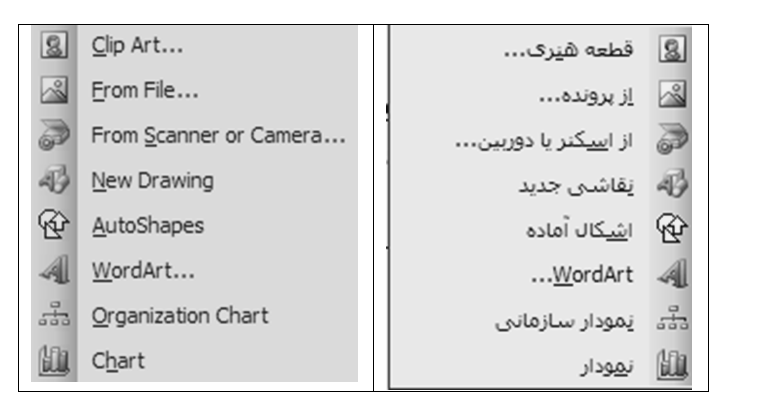
- برای درج برخی شکلهای آماده و موجود در خود برنامه بايد گزينه Clip Art را كليك كرده و شكل دلخواه را در كادر بعد انتخاب سازيم.
- براي درج يك تصوير از درايوهاي مختلف ديسك، فلاپي و Cd بايد:
Insertمنوي è Picture گزينهèFrom File… گزينه
- در ج نمودار در سند:
Insert منوي è Picture گزينه èChart گزينه
- درج نمودار سازماني در سند:
Insert منوي è Picture گزينه èOrganization Chart گزينه
- درج موضوعات ديگر مثلاً Media Clip :
Insert منوي è Object… گزينه èموضوع موردنظر
اگر قصد داشته باشيم تصاوير و موضوعات درج شده را تغيير اندازه دهيم، ابتدا آن موضوع را كليك نموده و سپس به كمك نقاط كليدي گوشه هاي آن، اندازه اي دلخواه را براي آن شكل،تنظيم مي كنيم.
1-26 آشنايي با چگونگی تنظيم قرار گرفتن متن و تصوير
با راست كليك روي شكل درج شده، و انتخاب گزينه Format… ، كادري نمايان مي شود كه در آن كادر مي توان چگونگي قرار گرفتن متن سند و تصوير را تعيين نمود. (توسط برگهLayout )

1-27 آشنايي با اضافه کردن کادر به سند و تنظيمات كادرها و سايه ها
از طريق منوی Format و گزينه Borders And Shading برنامه مربوط به تنظيمات كادرها و سايه ها (Borders And Shading) را ظاهر می سازيم. اين برنامه داراي سه برگه است:
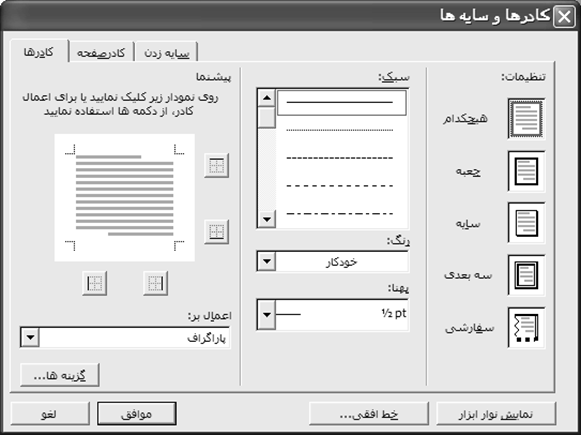
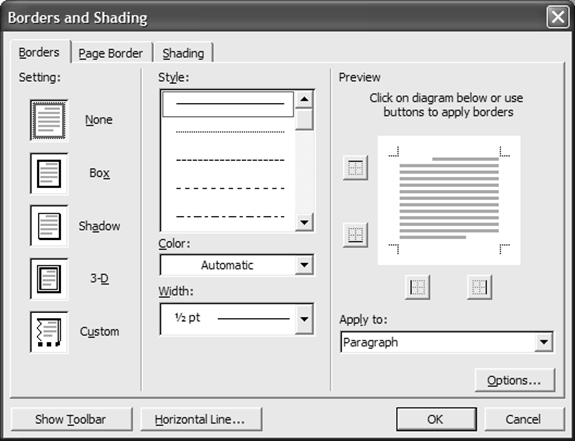
– برگه Borders : برای تنظيم نوع، رنگ و عرض خطوط جدول و همچنين تنظيم کادر در اطراف متن به کار می رود.
– برگهPage Border : برای تنظيم يك كادر و حاشيه براي كل صفحه می باشد.
– برگه Shading : برای تغيير رنگ زمينه و سايه زدن خانه هاي انتخاب شده استفاده می شود.
1-28 آشنايي با استفاده از مجموعه های مختلف چند فاصله (Tab)
برای تنظيم فاصله و پرش كليد Tab مي توان روي دكمه كوچكِ گوشه راست يا چپِ خط كش كليك نموده و نوع Tab را ، تعيين ساخت و سپس در جايي از خط كش كليك كرد تا فاصله پرشTab نيز تنظيم گردد.
اين دكمه ها عبارتند از:
چپ چين (Left Tab)
وسط چين(Center Tab)
راست چين(Right Tab)
مرتب نمودن نوشته هاي آن ستون با توجه به مميز اعشار(Decimal Tab)
خط جداكننده (Bar Tab)
راه ديگر اين است كه از منوي Format گزينه Tabs… را انتخاب كنيم.
| تعيين ميزان پرش كليد Tab |
| تعيين نحوه قرار گرفتن و مرتب شدن متني كه پس از فشردن كليد Tab تايپ خواهد شد. |
| تعيين نوع خط راهنماي Tab(فاصله Tab اول تغيير كرده ومثلاً نقطه چيني خواهد شد) |
| تعيين ميزان پيش فرض و اوليه پرش كليد Tab |
| ذخيره Tab |
@ به عنوان مثال در شكل بعد، ابتدا چند نوع Tab متفاوت ساخته و سپس شروع به تايپ متن نموده و براي اعمالِ فاصله از كليد Tab در صفحه كليد استفاده نمودهايم.
| A |
| B |
| C |
| D |
| E |
A – چپ چين B – راست چين C – وسط چين
D – خط فاصل E – اعشار
1-29 آشنايي با پيش نمايش چاپ (Print Priew)
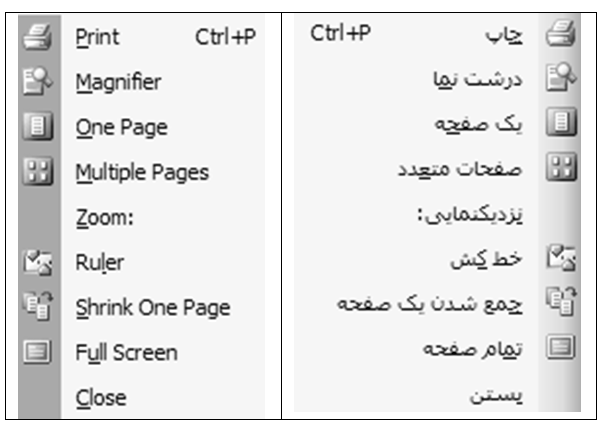
روي نوار ابزار استاندارد دكمه را كليك نموده ويا گزينه Print Preview را از منوي File انتخاب مي كنيم. در حالت پيش نمايش چاپ، نوار ابزار زير نمايان خواهد شد:
A – براي چاپ سند (Print) اين مورد را انتخاب مي كنيم.
B – ابزار بزرگ نمايي ( اگر فعال نباشد، مي توان در اين حالت نمايشي ، سند را ويرايش نمود.)
C – براي اين كه يك صفحه مشاهده شود، از اين گزينه استفاده مي شود.
D – براي اين كه چند صفحه مشاهده شود، از اين گزينه استفاده مي شود.
E – برای تنظيم درصد بزرگ نمايي استفاده می شود.
F – برای نمايش يا عدم نمايش خط كش می باشد.
G – برای جمع و جور نمودن سند (با حذف فضاهاي خالي زايد و با تغيير اندازه برخي مطالب) از اين گزينه استفاده مي شود.
H – برای نمايش تمام صفحه سند می باشد.
I– برای بستن اين حالت نمايشي و برگشت به حالت نمايشي معمولي از اين گزينه استفاده مي شود. ( كليد Esc )
J – نمايش اطلاعاتي درباره وضعيت قالب بندي متني كه با كليك مشخص مي نماييم.
1-30 آشنايي با تنظيمات صفحه و حاشيه سند
مي توان از طريق گزينه Page Setup از منوي File تنظيمات مهمي را براي چاپ انجام داد. كادر باز شده داراي 3 برگه مربوط به حاشيهها، كاغذ و چيدمان بوده كه به شرح هر يك ميپردازيم:
1-30-1 برگه Margins
هنگامي كه شروع به تايپ مي نماييم، از لبه كاغذ شروع نكرده بلكه يك مقدار فاصله از بالا، راست ، چپ و پائين بطور خودكار ايجاد مي گردد. اين بدين معني است كه در قسمتهـــاي كناري كاغذ (حاشيه) چيزي تايپ نمي شود.
در اين برگه مي توان فواصل و حاشيه هاي طرفين صفحه را تنظيم نمود و همچنين جهتِ چاپِ كاغذ را تعيين ساخت كه مطالب در طول كاغذ ويا در عرض آن چاپ شوند.


| تعيين جهت كاغذ (مطالب در طول كاغذ چاپ شوند يا در عرض آن) تنظيم فواصل و حاشيه هاي طرفين صفحه ( مثلاً متن سند نسبت به لبه بالايي كاغذ چقدر فاصله داشته باشد) |
1-30-2 برگه Paper
در اين برگه تعيين نوع و اندازه ابعاد كاغذ امكان پذير است. (مثلاً كاغذ A4)


1-30-3 برگه Layout
در اين برگه مي توان تنظيم نمود كه صفحه اولِ يك سندِ چند صفحه اي، سرصفحه، پاصفحه و شماره صفحه نداشته باشد همچنين اينكه سرصفحه و پاصفحه مربوط به صفحاتِ زوج و فرد با هم متفاوت باشد. در برگه Layout اين كادر، گزينه براي اين است كه سرصفحه و پاصفحه در صفحات زوج و فرد فرق داشته باشند. اگر اين گزينه را علامت نزنيم، سرصفحه و يا پا صفحه هاي صفحات زوج و فرد همانند يكديگر خواهند بود، مثلاً اگر در صفحه 1 كلمه “آنزان ” را به عنوان سرصفحه و يا پا صفحه تايپ كنيم ، اين كلمه عيناً در تمام صفحات زوج و فرد تكرار ميگردد. اما اگر گزينه فوق را تيك بزنيم، در اينصورت سرصفحات و يا پا صفحات ، زوج با فرد متفاوت خواهند بود، يعني اينكه ميتوان براي صفحات زوج يك سرصفحه و يا پا صفحه و براي صفحات فرد سرصفحه و يا پاصفحه ديگري تنظيم نمود.
و در همين برگه، گزينه اگر علامت دار باشد، آنگاه صفحه نخست سند، سر صفحه و پاصفحه نخواهد داشت. به عبارتی ديگر می توان تنظيم نمود که سرصفحه و پاصفحه در صفحه نخست متفاوت با بقيه صفحات باشد.
1-30-4 شناسايي اصول چاپ سند (Print)
روي نوار ابزار استاندارد دكمه را كليك نموده ويا گزينه Print… را از منوي File انتخاب مي كنيم. (با فشردن كليدهاي Ctrl + P نيز مي توان اين عمليات را انجام داد)
اگر چاپگر آماده بوده و مشكل خاصي وجود نداشته باشد، آنگاه تمامی صفحات سند فعلي بطور كامل به چاپ خواهند رسيد.
1-30-4-1 آشنايي با گزينه های اصلی چاپ
در صورتيكه از منوي File گزينه Print… را انتخاب كنيم، كادري ظاهر شده و به ما امكانات و اختيارات زيادي را در چاپ، ارايه مي نمايد.
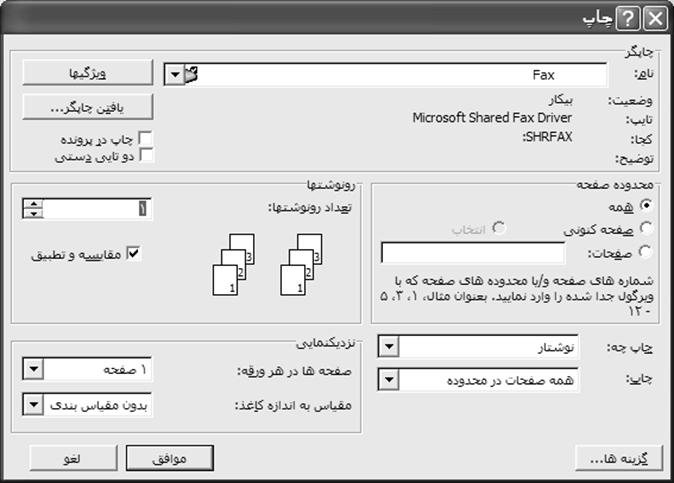
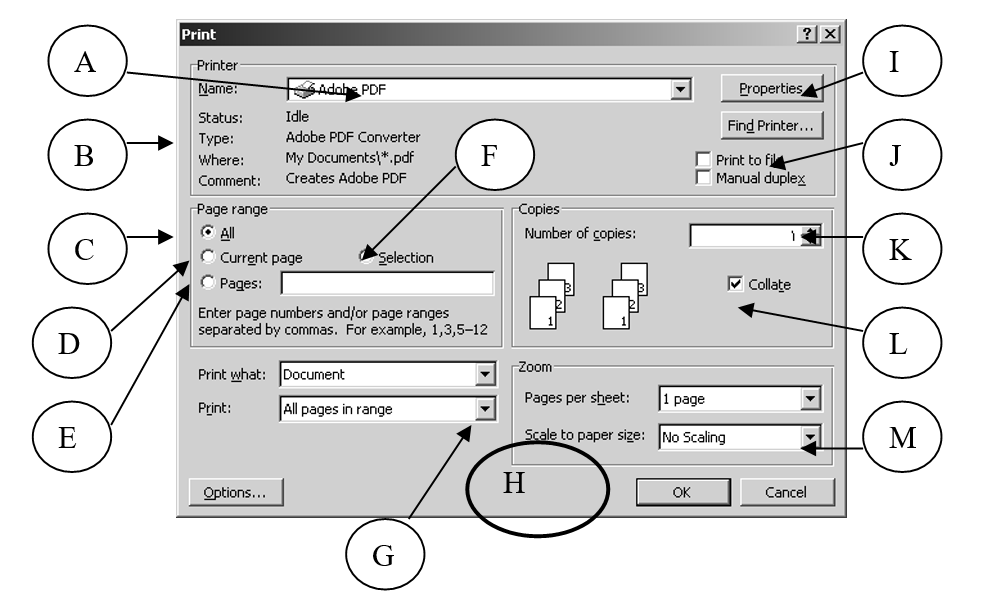
A– برای انتخاب نوع چاپگر می باشد. مثلاً در صورتي كه در يك سيستم، نوعي چاپگر ليزريِ سياه وسفيد و همچنين يك چاپگر رنگي نصب باشد، از اين ليست بازشونده قادر خواهيم بود، چاپگر دلخواه را انتخاب نماييم.
B– اطلاعاتي درباره چاپگر نمايش می دهد.
C– برای اين که همه صفحات سند چاپ شوند.
D– فقط صفحه فعلي (كه مكان نما در آنجاست) چاپ شود.
E– صفحات خاصي چاپ گردند مثلاً صفحات: 1,3,5-12 (يعني صفحات اول و سوم و صفحات پنجم تا دوازدهم به چاپ رسند)
F– فقط متنی که هم اکنون در حالت انتخاب است چاپ شود.
G– تعيين اينكه همه صفحات چاپ شوند يا فقط صفحات فرد و يا فقط صفحات زوج
H– برای چاپ نهايي سند استفاده می گردد.
I– برای تنظيم خصوصيات چاپگر در صورت لزوم استفاده می شود.
J– برای چاپ سند درون يك فايل مخصوص و ذخيره آن روي ديسك استفاده می شود.
K– تعيين تعداد نسخه اي كه مي خواهيم به چاپ رسد (تعداد كپي)
L– هنگام چاپ يك سند چند صفحه اي در چند سري، مي توان تنظيم نمود كه :
الف) تمام صفحات يك سري بطوركامل چاپ شوند و بعد يك سري ديگر و بعد …
(هر گاه گزينه Collate علامت دار باشد)
ب) ابتدا صفحه نخست به تعداد لازم به چاپ رسد و بعد صفحه دوم و بعد …
(هر گاه گزينه Collate علامت دار نباشد)
M– چاپ سند در صفحه اي با مقياس ديگر(چنين امكاني در دستگاههاي فتوكپي نيز وجود دارد)
با توجه به آشنايي با كادر مخصوص چاپ مي توان اين موارد راتنظيم نمود: تعيين نام چاپگري كه مي خواهيم اين سند را چاپ نمايد (در صورت داشتن چند چاپگر متفاوت)، تعدادكپي(چاپ) از صفحات (Number Of Copies ) در اين قسمت با انتخابAll تنظيم مي كنيم كه تمامي صفحات سند را از صفحه اول تا آخر چاپ نمايد و با انتخاب Current Page فقط صفحه اي كه همينك مكان نما در آن است،و فعال است را چاپ نمود و …
1-31 شناسايي اصول انتخاب الگوی مناسب (Template)
Word داراي الگوهاي تعريف شده براي بسياري نامه هاي اداري و تجاري ، صفحات اوليه فاكس، توضيحات و غيره مي باشد . ما ميتوانيم الگوهاي خاص خود را ايجاد كرده و يا الگوهاي موجود را بدلخواه تغيير داده و اصلاح نماييم. براي استفاده از يك الگوي موجود مي بايست از منـــوي File گزينه New را انتخاب نمود و در سمت راست ليست وظيفه ظاهر شده ، گزينه On My Computer را انتخاب كرد تا کادر مربوط ظاهر گردد و نهايتاً در سربرگ دلخواه از اين کادر، گزينه اي از موارد موجود را انتخاب ساخته و گزينه Document را در ناحيه پايين به انتخاب در آورده و دكمه Ok كليك كرد. اگر به جاي Document گزينه Template را انتخاب كنيم،الگوي جديدي ساخته خواهد شد.
براي ايجاد الگوي جديد، روش ديگر ايناست كه ابتدا سند مورد نظر را تايپ و ويرايش نموده و سپس از منوي File گزينه Save As را انتخاب نمود و از ليست باز شونده Save As Type در قسمت پايين، گزينه Document Template را انتخاب نمود.
1-32 آشنايي با بکار بردن يک شيوه يا سبك (Style)
سبك مجموعه اي از قالب بنديها براي اعمال بر روي متون بصورت يكجا مي باشد. براي استفاده از يكي از انواع سبك موجود در ابتداي نـــوار ابزار Formatting روي فلش رو به پائين Style كليك مي كنيم تا ليستي از سبك ها مشاهده شوند.
از اين ليست سبك مورد نظر را با كليك كردن روي نام آن، انتخاب مي نماييم تا اين سبك به متن انتخاب شده اعمال شود. براي ايجاد سبك جديد از منوي Format گزينه Styles And Formatting راكليك نموده و دكمه را انتخاب مي كنيم تا كادر محاوره اي New Style ظاهر شود، سپس در قسمت Name نام سبك جديد را وارد مي كنيم و در قسمت پايين دكمه Format راكليك كرده و قالب بندي و تغييرات دلخواه را از گزينه هاي مشاهده شده انتخاب كرده (مثلاً گزينه Font ) و Ok راكليك مي كنيم.
1-33 آشنايي با اصول عمليات ادغام پستي (Mail Merge)
گاهی لازم است که نامه ای با متن واحد (ولی با ذکر برخی اطلاعات مربوط به گيرنده نامه) به تعداد زياد و براي چند نفر ارسال شود. در اين هنگام از برنامه ادغام پستی Ms-Wordاستفاده می کنيم، اين برنامه برای تکثير نامه ها و يا برچسب و كاتالوگ كمك شاياني در اختيار قرار می دهد.
برنامه ادغام پستی از سه جزء تشکيل می شود. نامه فرم (شامل متن مشترک نامه ها می باشد)، منبع داده (فايلی که حاوی اطلاعات متغير می باشد) و فيلد ادغام (تنظيمات تعيين کننده اين که کدام اطلاعات متغيير در چه جايي از متن نامه قرار گيرد)
در اينجا با استفاده از راهنمای قدم به قدم برنامه ادغام پستی Ms-Wordيک نامه تبريک را برای ارسال به دوستان خود تنظيم می کنيم. براي اين منظور به روش زير عمل مي نماييم:
1. از منوی Toolsگزينه Letters And Mailings و سپس گزينه Mail Merge را انتخاب می کنيم. ليست مخصوص اين فرمان نمايان خواهد شد:
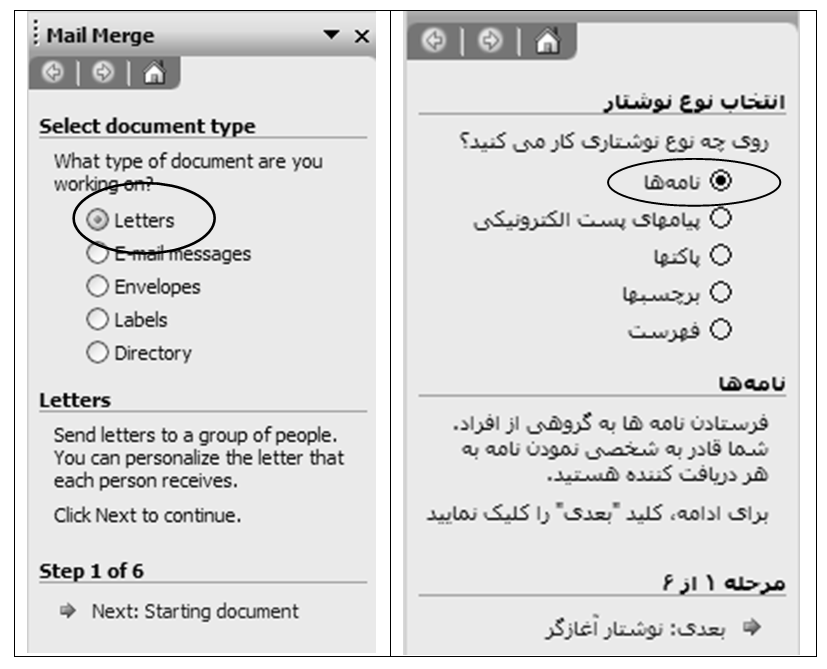
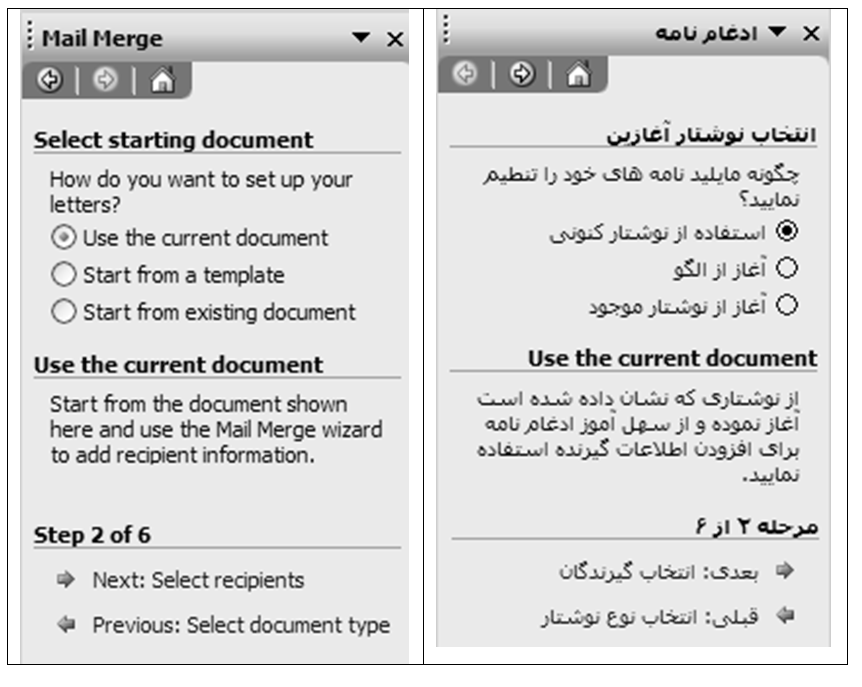
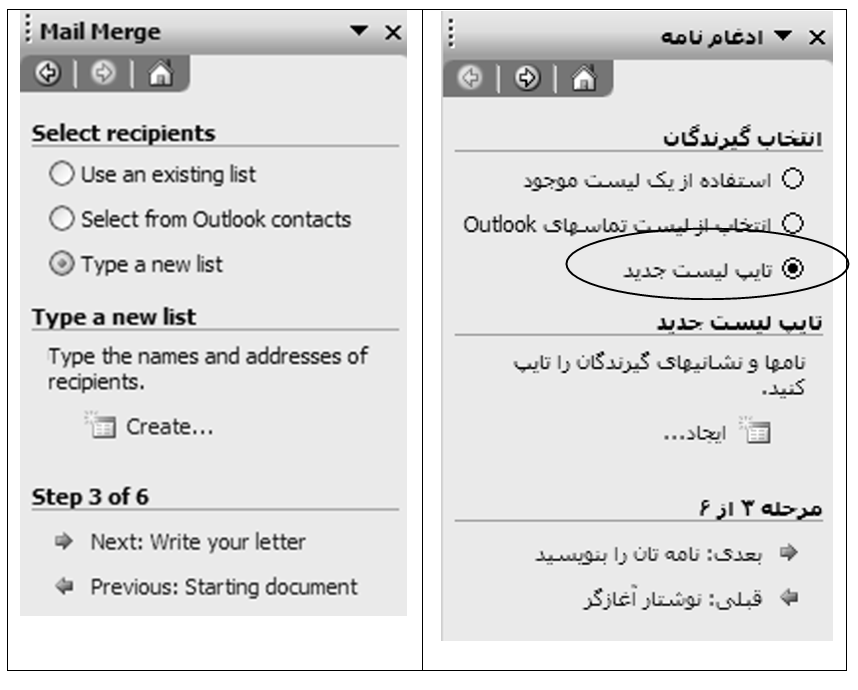
مورد دلخواه را از اين ليست انتخاب نموده و براي انجام عمليات ادغام، گزينه را كليك می نماييم.
2. از كادر بعد گزينه نخست را انتخاب مي نماييم:
گزينه را كليك می نماييم.
3. اگر ليست گيرندگان نامه را در گذشته تهيه و تنظيم نکرده باشيم، گزينه سوم را از ليست بعدی انتخاب می کنيم.
4. گزينه Create را در همين ليست انتخاب می کنيم تا کادر New Address List ظاهر شود. سپس به تايپ مشخصات گيرنده های نامه می پردازيم.
برای ايجاد يک رکورد جديد و درج مشخصات گيرنده ديگر نامه از دکمه New Entry کمک می گيريم. و برای تغيير اساسی بانک اطلاعاتی خود، دكمه Customize را انتخاب نموده و بانك اطلاعاتي خود را به دلخواه تنظيم می كنيم. در اينصورت كادري ظاهر شده و به ما اين امكان را مي دهد كه فيلدهاي بانك اطلاعاتي را تغيير دهيم (ايجاد، حذف، تغييرنام و …)
5. کادر New Address List را می بنديم. در اين صورت کادر Save ظاهر خواهد شد که در اين کادر نامی را برای سند تعيين نموده و آن را ذخيره می کنيم.
6. کادر بعدی نمايان شده و امکان اعمال تنظيمات ديگری را در اختيار قرار می دهد.
تغييرات دلخواه را انجام داده و کادر را تاييد نموده و سپس گزينه Next را در پايين ليست وظيفه كليك می نماييم.
7. در ليست بعد کادر مربوط به تعيين نوع نامه ظاهر خواهد شد که يکی از گزينه ها را انتخاب کرده (مثلاً Greeting Line) و Next را کليک می کنيم.
8. در کادر بعد پيش نمايش يکی از نامه ها را مشاهده نموده و در صورت لزوم تغيرات دلخواه را اعمال کرده و دکمه Next را کليک می کنيم.
9. کادر مربوط به آخرين عمليات ادغام نمايش داده خواهد شد.
نهايتاً براي انجام نهايي عملياتِ ادغام و مشاهده نتيجه ، يكي از گزينه هاي زير را انتخاب مي كنيم:
1-34 مفهوم Book Mark
مي توان محلي در سند را براي مراجعات بعدي و انتقال سريع اشاره گر به آن، نامگذاري (علامت گذاری) نمود. به اين نام و علامت ها Book Mark گويند. براي ايجاد Book Mark ابتدا اشاره گر را به محل دلخواه از سند منتقل نموده و بعد از منوي Insert گزينه Book Mark را انتخاب مي كنيم و در قسمت Book Mark Name نامي را تايپ كرده(نام بايد با يك حرف الفبا آغاز شود) و دكمه Add راكليك مي كنيم. براي استفاده از Book Mark و انتقال اشاره گر به محل دلخواه به توضيحات 8-1 قسمت Go To رجوع شود.
1-35 پاكت نامه ها و برچسب ها(Envelopes And Labels )
از منويTools و منوي فرعي Letters And Mailings مي توان برنامه Envelopes And Labels را اجرا كرد و در برگه هاي مربوط، در قسمت مشخص شده، متن دلخواه را براي پاكت نامه ها و برچسب ها تنظيم نمود.
1-36 شمارش كلمات(Word Count…)
مي توان از برنامه Word گزارشي از تعداد صفحات،كلمات،كاراكترها و… را درخواست نمود. براي اين كار از منوي Tools گزينه Word Count.. را انتخاب مي كنيم.
1-37 اعمال كلمه رمز
در كادر Save As مي توان براي سند فعلي خود يك رمز تهيه نمود تا ديگران بدون آن كلمه رمز نتوانند آن سند را باز نموده و يا ويرايش كنند. با توجه به شكل بعد بايد در كادر Save As از منوي Tools گزينه Security Options را اجرا نمود و سپس Password را در قسمت Open يا Modify تايپ نمود.
1-38 ايجاد يادداشت(Comment)
مي توان تنظيماتي ايجاد نمود كه هرگاه اشاره گر ماوس در محل دلخواه از سند، قرارگيرد، يك يادداشت در كادري زردرنگ نمايان شود. روش ايجادِ يادداشت به اين صورت است كه ابتدا ماوس را در محل دلخواه از سند قرار مي دهيم، آنگاه از منوي Insert گزينه Comment را برگزيده ودر كادر بازشده توضيح مورد نظر را تايپ مي نماييم.
1-39 ستون بندي متن (Columns)
براي چند ستوني ويا روزنامه اي نمودن متن، دكمه Columns را از نوار ابزار استاندارد انتخاب نموده و تعيين مي سازيم كه سند فعلي چند ستوني باشد. در ضمن توسط گزينه Columns از منوي Format مي توان كادر مخصوص اين عمليات را ظاهر ساخت و تنظيمات دلخواه را در آن انجام داد. به عنوان مثال سند دوستوني شده و بين ستونها خط جدا كننده قرار گيرد. (گزينهLine Between را علامت مي زنيم تا بين ستونها خط جدا كننده قرار گيرد)
سند دوستوني با خط جداكننده بين ستونها
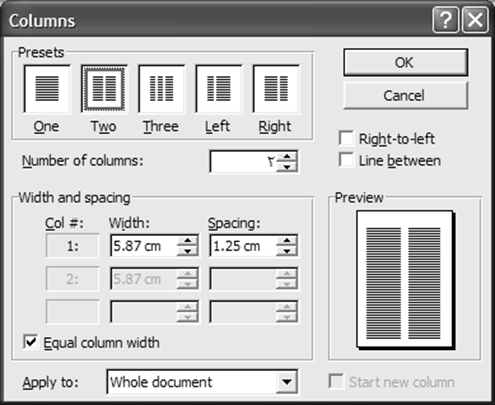
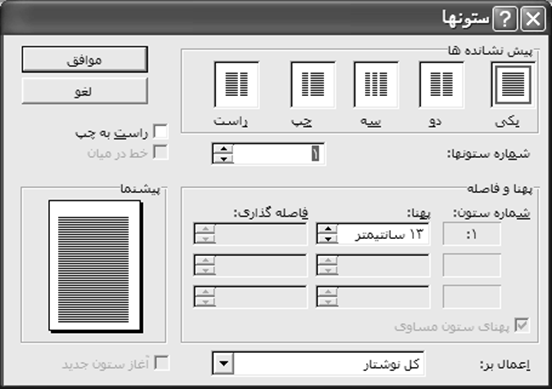
1-40 انتقال قالب بندي(Format Painter)
گاهي در يك سند، قالب بندي هاي متفاوتي ملاحظه مي شود مثلاً يك كلمه داراي رنگ و اندازه خاصي باشد. اگر ما بخواهيم چند كلمه ديگر را در متن، دقيقاً به فرمت كلمه موردنظر درآوريم، آنگاه به ترتيب زير عمل مي كنيم:
- روي كلمه نمونه كليك مي كنيم.
- دكمه در نوار ابزار استاندارد را دابل كليك مي نماييم.
- روي كلمه يا كلماتي كه مي خواهيم شبيه كلمه نمونه شوند، كليك مي كنيم.
اگر يك بار كليك نماييم فقط يك دفعه قابل استفاده بوده ولي اگر بخواهيم چندين بار از اين امكان استفاده نماييم، بايد دو بار بطور سريع و متوالي روي اين دكمه كليك كنيم
و هر گاه بخواهيم آنرا از فعاليت بيندازيم، مجدداً روي آن كليك مي نماييم.
1-41 برنامه Find
براي جستجوي يك عبارت در سند فعلي كاربرد دارد. گزينه Find از منوي Edit ، كادر مخصوص اين فرمان را نمايان مي سازد. عبارت مورد جستجو را در قسمت مشخص شده تايپ كرده و كليد Enter ( يا دكمه Find Next ) را انتخاب مي كنيم. كلمه مورد نظر، يافته شده و پر رنگ ميشود. بازدن دكمه (Find Next ) آن كلمه را در سطرهاي بعدي نيز مي يابد.
مثال) جستجوي عبارت “سرزمين ” در سند فعلي:
1. در قسمت بالايي كادر اين برنامه، متن مورد نظر را تايپ مي كنيم.
2. دكمه Find Next را انتخاب مي كنيم.
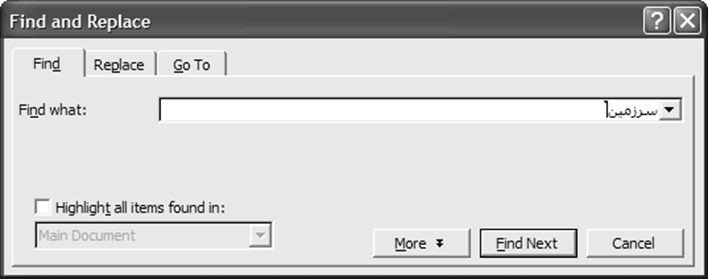
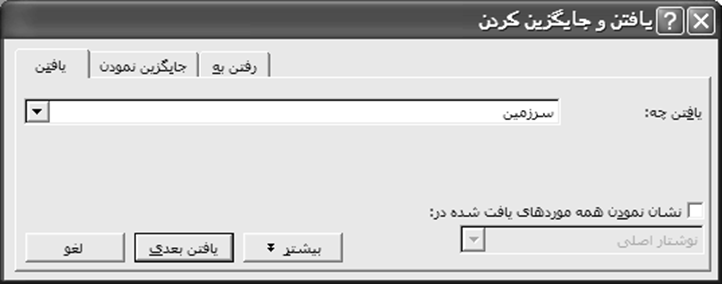
| 1 2 |
1-42 برنامه جايگزينی کلمات (Replace )
اگر بخواهيم كلمه اي را در متن سند خود يافته و با كلمه اي ديگر عوض كنيم، در برگه Replace (با توجه به شكل بعد) براي جايگزيني عبارت جديد به جاي عبارت موجود تنظيمات لازم را انجام مي دهيم. براي مثال عبارت جديد “شادمان” را جايگزين همه عبارات قبلاً موجودِ “اندوهگين” مي كنيم:
1. در قسمت بالايي اين برگه، عبارت و كلمه اي موجود در متن سند را درج مي كنيم.
2. در قسمت پايين اين برگه، عبارتي جديد تايپ مي كنيم تا جايگزين عبارت قبلي شود.
3. دكمه Replace را براي تغيير اولين مورد يافته شده كليك نموده و يا اينكه دكمه Replace All را براي جايگزيني عبارت جديد به جاي تمامي عبارات تعيين شده انتخاب مي نماييم.
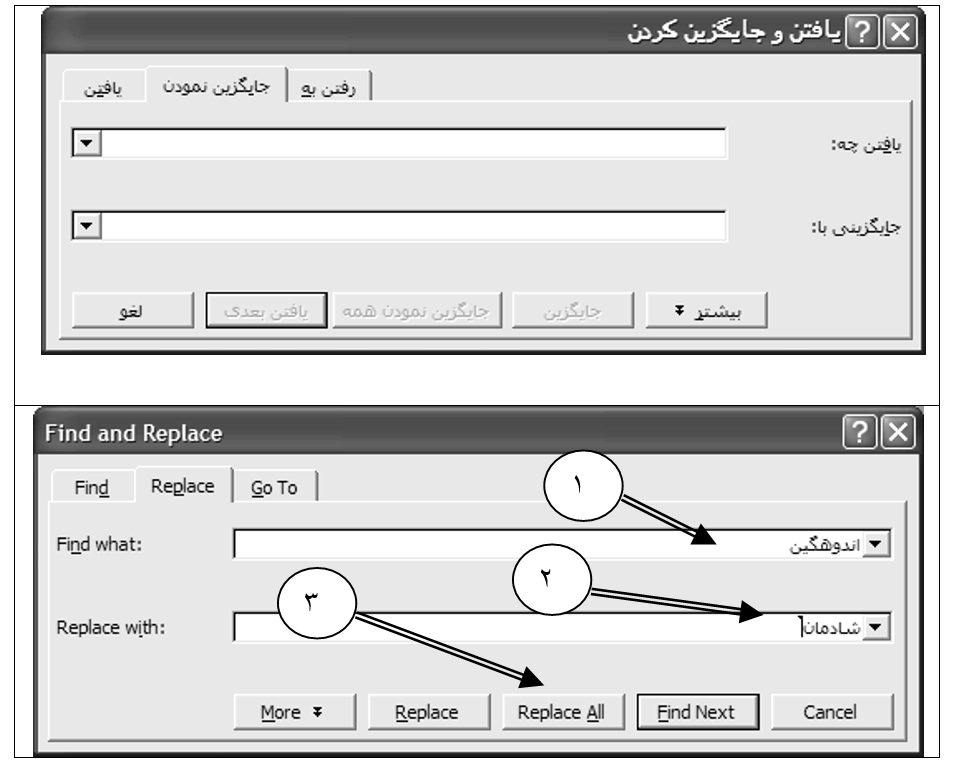
| 1 2 3 |
1-43 آشنايي با نحوه جابجايي سريع مکان نما در سند (Go To)
در برگه سوم اين كادر (Go To)، مي توان مكان نما را به محل دلخواه از سند، مثلاً صفحات، بخشها، خطوط، علايم، جدولها و… منتقل ساخت.. به عنوان نمونه، در يك سند چند صفحه اي مكان نما (اشاره گر) را به صفحه 7 انتقال مي دهيم:
1. در ليست سمت چپ اين برگه تعيين مي كنيم كه اشاره گر به كجاي متن پرش نمايد. مثلاً گزينه Page را انتخاب مي كنيم.
2.در قسمت مقابل اين گزينه با تا يپ در محدوده مشخص شده، تعيين مي كنيم كه اشاره گر به كجاي سند (كدام صفحه) جابجا شود.
3. دكمه Go To را كليك مي كنيم.
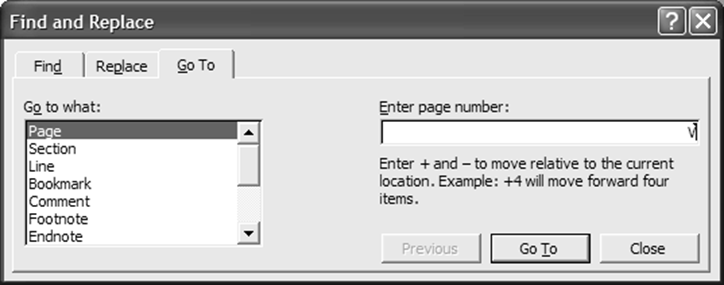
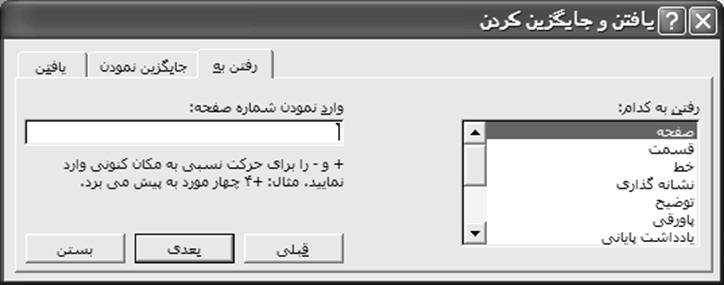
1-45 برخي كليدهاي ميان بر مربوط به برنامه Microsoft Office Word
| باز نمودن سند موجود CTRL+O ايجاد سند جديد CTRL+N ذخيره مجدد سند F12 ذخيره سند CTRL+S پيش نمايش چاپ CTRL+F2 چاپ CTRL+P تصحيح املايي و دستوري F7 يافتن عبارت در متن سند CTRL+F جايگزيني CTRL+H انتقال مكان نما به محل دلخواه CTRL+G انتخاب كل سند CTRL+A انتخاب تا ابتداي سطر SHIFT+Home انتخاب تا انتهاي سطر SHIFT+END انتقال به ابتداي سطر HOME انتقال به انتهاي سطر END انتقال به ابتداي سند CTRL+Home انتقال به انتهاي سند CTRL+End Cut CTRL+X Copy CTRL+C Paste CTRL+V Undo CTRL+Z Redo CTRL+Y چپ چين CTRL+L وسط چين CTRL+E راست چين CTRL+R منوي راست كليك SHIFT+F10 حذف قالب بندي فعلي متن انتخاب شده Ctrl+Shift+N | حذف كلمه قبلي CTRL+Backspace علامت گذاري ليست CTRL+SHIFT+L ايجاد صفحه جديد CTRL+Enter زير خط CTRL+U دو زير خط CTRL+SHIFT+D يزرگي حروف CTRL+SHIFT+A بزرگ يا كوچكي حروف SHIFT+F3 پايين نويس CTRL+ = بالا نويس CTRL+SHIFT+= تغيير نوع قلم CTRL+SHIFT+F تغيير اندازه قلم CTRL+SHIFT+P افزايش اندازه قلم CTRL+] كاهش اندازه قلم CTRL+[ مخفي نمودن متن CTRL+SHIFT+H مشاهده قالب بندي متونِ مختلفِ سند SHIFT+F1 كپي قالب بندي يك متن CTRL+SHIFT+C انتقال قالب بندي كپي شده به متن ديگر (حتي به سند ديگر) ! CTRL+SHIFT+V فاصله معمولي بين سطرها CTRL+1 دو برابر شدن فاصله CTRL+2 يك و نيم برابر شدن فاصله بين سطرها CTRL+5 حذف قالب بندي پاراگراف CTRL+Q |
بخش دوم
۳- اینترنت ICDL۳- اینترنت ICDL
آموزشگاه هوش مصنوعی
۳۰ مورد مبانی و مفاهیم اولیه مربوط به آموزش اینترنت
1- مفاهیم پایه اینترنت
- تعریف اینترنت و تفاوت آن با شبکههای محلی (LAN, WAN)
- آشنایی با مفهوم مرورگر وب (Browser) و انواع آن (Chrome, Firefox, Edge)
- تعریف URL و بخشهای آن (پروتکل، دامنه، مسیر(: https://whatismyipaddress.com
- مفهوم موتور جستجو (Google, Bing, Yahoo) و نحوه استفاده از آن
- معرفی وبسایت و تفاوت آن با وبپیج
- آشنایی با ایمیل و نحوه ایجاد یک حساب ایمیل (Gmail, Yahoo)
- تعریف مفهوم دانلود و آپلود فایل
- مفهوم لینک (Hyperlink) و نحوه استفاده از آن
- معرفی پروتکلهای اصلی (HTTP, HTTPS)
- تعریف شبکههای اجتماعی و نمونههایی از آنها (Facebook, Instagram, Twitter)
2- ارتباط و امنیت در اینترنت
- مفهوم آدرس IP و نحوه کارکرد آن
- معرفی DNS و نقش آن در ترجمه آدرسها
- آشنایی با Wi-Fi و شبکههای بیسیم
- تعریف VPN و کاربرد آن در امنیت و دسترسی
- اهمیت رمزگذاری (Encryption) در اینترنت
- روشهای ایمنسازی اطلاعات شخصی در اینترنت
- مفهوم کوکیها و استفاده از آنها توسط وبسایتها
- شناسایی وبسایتهای امن) قفل سبز – HTTPS)
- اصول مدیریت رمز عبور و استفاده از ابزارهای مدیریت رمز
- مفهوم فیشینگ و نحوه جلوگیری از آن
3- ابزارها و خدمات اینترنتی
- استفاده از سرویسهای ذخیرهسازی ابری (Google Drive, Dropbox)
- معرفی و نحوه استفاده از نقشههای آنلاین (Google Maps)
- مفهوم استریمینگ و خدمات آن (YouTube, Netflix)
- نحوه خرید آنلاین و پرداختهای اینترنتی
- معرفی موتورهای جستجوی تخصصی (Scholar, DuckDuckGo)
- آشنایی با پیامرسانها (WhatsApp, Telegram)
- استفاده از ابزارهای کنفرانس آنلاین (Zoom, Microsoft Teams)
- نصب و مدیریت افزونههای مرورگر
- آشنایی با قوانین رفتار آنلاین (نتیکت)
- شناسایی تهدیدات اینترنتی (بدافزارها، هک، جاسوسافزار)
آموزشگاه هوش مصنوعی: ۳۰ مورد مبانی و مفاهیم اولیه مربوط به آموزش اینترنت
1– مفاهیم پایه اینترنت:
- اینترنت شبکهای جهانی است که با شبکههای محلی (LAN) و گسترده (WAN) تفاوت دارد.
- مرورگر وب نرمافزاری برای دسترسی به اینترنت است؛ نمونهها: Chrome، Firefox، Edge.
- URL نشانی وب است که شامل پروتکل، دامنه و مسیر است؛ مثال: https://whatismyipaddress.com.
Hypertext Transfer Protocol – World Wide Web
- موتور جستجو ابزاری برای یافتن اطلاعات در وب است؛ نمونهها: Google، Bing، Yahoo.
- وبسایت مجموعهای از صفحات وب مرتبط است؛ وبپیج یک صفحه از وبسایت است.
- ایمیل یک روش ارتباطی دیجیتال است؛ با خدماتی مثل Gmail، Yahoo میتوان حساب ساخت.
- دانلود به معنی دریافت فایل و آپلود به معنی ارسال فایل به سرور است.
- لینک یا Hyperlink، اتصال به یک صفحه وب دیگر است.
- پروتکل HTTP و HTTPS نحوه تبادل اطلاعات بین مرورگر و سرور را تعیین میکنند.
- شبکههای اجتماعی، پلتفرمهایی برای ارتباط و اشتراک محتوا هستند؛ نمونهها: Facebook، Instagram.
2– ارتباط و امنیت در اینترنت:
- آدرس IP شناسه دستگاه در شبکه اینترنت است. Internet Protocol
- DNS وظیفه ترجمه نام دامنه به آدرس IP را بر عهده دارد.
- Wi-Fi یک فناوری بیسیم برای اتصال به اینترنت است.
- VPN ارتباط امن و خصوصی در اینترنت ایجاد میکند و دسترسی را تسهیل میکند.
- رمزگذاری دادهها را از دسترسی غیرمجاز محافظت میکند.
- ایمنسازی اطلاعات شامل استفاده از رمزهای قوی و مدیریت حریم خصوصی است.
- کوکیها فایلهای کوچک ذخیرهشده توسط برخی وبسایتها هستند. برای این که کاربرها بتوانند در بازدیدهای بعدی راحتتر عمل کنند.
- وبسایتهای امن با HTTPS و قفل سبز مشخص میشوند.
- مدیریت رمز عبور با استفاده از ابزارهایی مثل LastPass امنیت را افزایش میدهد.
- فیشینگ تلاشی برای سرقت اطلاعات با تقلید از منابع معتبر است.
3– ابزارها و خدمات اینترنتی:
- ذخیرهسازی ابری به کاربران اجازه میدهد فایلهای خود را آنلاین ذخیره کنند؛ نمونهها: Google Drive.
- نقشههای آنلاین مثل Google Maps برای مسیریابی و اطلاعات مکان استفاده میشوند.
- استریمینگ، تماشای محتوا به صورت زنده یا آنلاین است؛ نمونهها: YouTube، Netflix.
- خرید آنلاین و پرداخت اینترنتی شامل انتخاب محصول و پرداخت امن است.
- موتورهای جستجوی تخصصی مثل Google Scholar اطلاعات علمی را ارائه میدهند.
- پیامرسانهایی مثل WhatsApp و Telegram ابزارهای ارتباطی فوری هستند.
- ابزارهای کنفرانس آنلاین مثل Zoom برای جلسات از راه دور استفاده میشوند.
- افزونههای مرورگر ویژگیهای مرورگر را گسترش میدهند. Extension
- نتیکت به معنای رعایت اصول اخلاقی در فضای آنلاین است.
- تهدیدات اینترنتی شامل بدافزارها، هک و جاسوسافزارهاست.
- باز کردن یک صفحه وب
تایپ آدرس وبسایت در نوار آدرس مرورگر و فشردن Enter.
- جستجو در گوگل
تایپ عبارت جستجو در نوار جستجوی گوگل و فشردن Enter. - باز کردن تب جدید در مرورگر
فشار دادن Ctrl+T. - باز کردن وبسایت در تب جدید
راستکلیک روی لینک –> Open link in new tab.
- ذخیره صفحه وب به عنوان PDF
فشار دادن Ctrl+P –> انتخاب “Save as PDF” –> Save.
- علامتگذاری یک صفحه وب به عنوان مورد علاقه
فشار دادن Ctrl+D یا کلیک روی آیکون ستاره در نوار آدرس. - وارد کردن پسورد در سایت
تایپ نام کاربری و پسورد در فیلدهای مربوطه و کلیک روی Login. - پاک کردن تاریخچه مرورگر
انتخاب تنظیمات مرورگر –> Privacy & Security –> Clear Browsing Data.
- استفاده از حالت ناشناس (Incognito)
فشار دادن Ctrl+Shift+N یا انتخاب گزینه New Incognito Window در منوی مرورگر.
- باز کردن وبسایت با استفاده از URL
تایپ آدرس کامل (URL) در نوار آدرس مرورگر و فشردن Enter. - اضافه کردن وبسایت به لیست خواندن (Reading List)
راستکلیک روی لینک –> Add to Reading List.
- استفاده از افزونهها (Extensions) در مرورگر
رفتن به تب Extensions در تنظیمات مرورگر و نصب افزونههای مورد نظر. - پخش ویدیو از سایت یوتیوب
تایپ www.youtube.com در نوار آدرس و جستجو برای ویدیو مورد نظر. - آپلود فایل به یک سایت (مثلاً گوگل درایو)
ورود به حساب کاربری –> کلیک روی گزینه Upload –> انتخاب فایل.
- بلاک کردن کوکیها در مرورگر
انتخاب تنظیمات مرورگر –> Privacy –> Block third-party cookies.
- تعویض موتور جستجو پیشفرض
انتخاب تنظیمات مرورگر –> Search Engine –> انتخاب موتور جستجوی دلخواه.
- ارسال ایمیل از طریق Gmail
ورود به حساب Gmail –> کلیک روی Compose –> وارد کردن ایمیل و ارسال.
- دانلود یک فایل از اینترنت
راستکلیک روی لینک دانلود –> Save Link As یا انتخاب گزینه Download.
- اشتراکگذاری یک لینک وبسایت
کپی کردن آدرس سایت از نوار آدرس و ارسال آن به دیگران.
- ارسال پیام در چت آنلاین (چت سایت)
تایپ پیام در کادر چت و فشردن Enter. - تغییر زبان سایت
انتخاب گزینه Language در پایین سایت یا در منو و انتخاب زبان دلخواه. - مشاهده سایت در حالت موبایل
راستکلیک روی صفحه –> Inspect –> انتخاب تب موبایل.
- بررسی امنیت سایت (https)
بررسی وجود قفل سبز رنگ در نوار آدرس مرورگر. - استفاده از جستجو در داخل یک صفحه وب
فشار دادن Ctrl+F و تایپ عبارت مورد نظر. - مقایسه قیمتها آنلاین
جستجو برای محصول در چندین وبسایت فروشگاه آنلاین. - پاک کردن کش مرورگر
انتخاب تنظیمات مرورگر –> Privacy & Security –> Clear Cache.
- افزودن صفحه به لیست مطالعه
کلیک روی آیکون ستاره در نوار آدرس و انتخاب Add to Reading List. - مشاهده تاریخچه مرورگر
فشار دادن Ctrl+H یا انتخاب گزینه History در منوی مرورگر. - فعال کردن یا غیرفعال کردن اعلانها
انتخاب تنظیمات مرورگر –> Notifications –> فعال یا غیرفعال کردن اعلانها.
- اشتراکگذاری صفحه وب در شبکههای اجتماعی
کلیک روی آیکون اشتراکگذاری در صفحه وب و انتخاب شبکه اجتماعی مورد نظر. - جستجو با استفاده از کلمات کلیدی در گوگل
تایپ کلمات کلیدی مرتبط با موضوع در نوار جستجوی گوگل و فشار دادن Enter. - جستجوی عبارت دقیق با استفاده از علامت نقل قول
تایپ عبارت مورد نظر در گوگل داخل علامت نقل قول – مثلاً "ماشینهای الکتریکی"
- جستجو برای سایت خاص با استفاده از دستور
site:
تایپsite:example.comکلمه جستجودر گوگل -مثلاًsite:bbc.com news - جستجوی در محدوده تاریخ مشخص با استفاده از ابزار تاریخ
پس از جستجو در گوگل، انتخاب گزینه “Tools” و سپس “Any time” برای فیلتر کردن نتایج براساس تاریخ. - جستجو برای فایلهای خاص با استفاده از دستور
filetype:
تایپfiletype:pdfعنوان جستجودر گوگل برای پیدا کردن فایلهای PDF مرتبط با جستجو. - جستجوی عکس مشابه با استفاده از گوگل ایمیجز
وارد Google Images شوید، روی آیکون دوربین کلیک کنید و تصویر را آپلود کنید تا مشابه آن پیدا شود. - جستجوی در شبکههای اجتماعی با استفاده از هشتگها
تایپ هشتگ (#) و کلمه کلیدی در نوار جستجوی شبکه اجتماعی (مثلاً #خلاقیت). - جستجو برای مقالات علمی با استفاده از Google Scholar
وارد Google Scholar شوید و کلمات کلیدی مرتبط با تحقیق را جستجو کنید. - جستجوی از طریق کلمات مترادف
استفاده از کلمات مترادف برای گسترش نتایج جستجو – مثلاً استفاده از “auto” به جای “car” - جستجوی دادهها در منابع خاص مانند کتابها
تایپbook:عنوان کتابدر گوگل برای جستجوی اطلاعات از کتابها. - استفاده از Google Trends برای بررسی محبوبیت جستجوها
وارد Google Trends شوید و برای تحلیل روند جستجوهای خاص استفاده کنید. - جستجوی موضوعات مشابه با استفاده از “Related:”
تایپrelated:example.comدر گوگل برای جستجوی سایتهای مشابه با سایت هدف. - جستجو برای فیلمها و ویدیوهای خاص در یوتیوب
تایپ عنوان یا کلمات کلیدی در نوار جستجوی یوتیوب. - جستجوی از طریق PDFهای آنلاین با استفاده از
filetype:pdf
تایپfiletype:pdfموضوع جستجودر گوگل برای جستجو در فایلهای PDF. - جستجو بر اساس مکان با استفاده از ابزار جستجوی گوگل
استفاده از ابزار “Location” در گوگل برای جستجوی نتایج خاص به منطقه جغرافیایی خاص. - استفاده از جستجوهای پیشرفته گوگل برای فیلتر کردن نتایج
وارد Google Advanced Search شوید و فیلترهای دلخواه خود را اعمال کنید. - جستجوی در مقالات خبری با استفاده از دستور
inurl:
تایپinurl:newsعنوان جستجوبرای پیدا کردن مقالات خبری مرتبط. - جستجو برای کدهای برنامهنویسی با استفاده از Stack Overflow
وارد Stack Overflow شوید و کلمات کلیدی برنامهنویسی را جستجو کنید. - جستجو برای کتابهای رایگان با استفاده از منابع قانونی آنلاین
استفاده از وبسایتهای مانند Project Gutenberg برای جستجوی کتابهای رایگان. - جستجو در انجمنهای آنلاین برای مشکلات خاص
وارد انجمنهای مربوطه مانند Reddit یا Quora شوید و سوالات مشابه را جستجو کنید. - جستجوی در منابع علمی و پژوهشی از طریق JSTOR یا ResearchGate
جستجوی مقالات علمی در JSTOR یا ResearchGate. - جستجوی URLهای مشخص با استفاده از
inurl:
تایپinurl:keywordبرای جستجوی URLهایی که کلمه کلیدی در آنها وجود دارد. - جستجوی فیلتر شده برای قیمتها در وبسایتهای خرید
استفاده از فیلترهای وبسایتهای خرید برای جستجوی قیمت و ویژگیهای کالا. - جستجوی خبرهای خاص در سایتهای خبری با استفاده از
site:
تایپsite:bbc.comاخبار روزبرای جستجوی اخبار در سایت خاص. - جستجو برای کتابها با استفاده از Google Books
وارد Google Books شوید و نام یا موضوع کتاب را جستجو کنید. - جستجو برای اطلاعات در سایتهای آموزش آنلاین
استفاده از منابع مانند Coursera یا edX برای جستجوی دورههای آموزشی. - جستجوی در دیتابیسهای تخصصی مانند PubMed
جستجو برای مقالات پزشکی در PubMed. - جستجو برای کتابهای الکترونیکی در کتابخانههای آنلاین
جستجو در Google Books یا Open Library برای یافتن کتابهای الکترونیکی. - جستجو با استفاده از اپلیکیشنهای موبایل برای محصولات خاص
استفاده از اپلیکیشنهای فروشگاهی مانند Amazon یا eBay برای جستجوی محصولات خاص. - جستجو برای رفرنسها و منابع در ویکیپدیا
جستجو برای موضوعات خاص در ویکیپدیا و مراجعه به منابع ذکر شده در انتهای مقاله.

تعریف ICDL مهارتهای هفتگانه کامپیوترتعریف ICDL مهارتهای هفتگانه کامپیوتر
تعریف ICDL مهارتهای هفتگانه کامپیوتر
ICDL مخفف International Computer Driving License به معنای «گواهینامه بینالمللی کاربری کامپیوتر» است. این استاندارد بینالمللی برای یادگیری مهارتهای اولیه استفاده از کامپیوتر طراحی شده و در هفت مهارت اصلی دستهبندی میشود.
مهارتهای هفتگانه ICDL
- مفاهیم پایه فناوری اطلاعات Basic Concepts of IT
آشنایی با مفاهیم اولیه فناوری اطلاعات، سختافزار، نرمافزار، شبکهها و امنیت دادهها.
مثال آشنایی با انواع کامپیوترها، سیستمعاملها، و کاربرد اینترنت. - استفاده از کامپیوتر و مدیریت فایلها Using Computer and Managing Files
آموزش نحوه کار با سیستمعامل مانند ویندوز، مدیریت فایلها و پوشهها، و آشنایی با تنظیمات اصلی سیستم.
مثال ایجاد پوشه، کپی و انتقال فایلها. - واژهپردازی Word Processing
استفاده از نرمافزارهای ویرایش متن مانند Microsoft Word برای ایجاد، ویرایش، و قالببندی اسناد.
مثال نوشتن نامه، ایجاد جدول و قالببندی متن. - صفحات گسترده Spreadsheets
کار با نرمافزارهایی مثل Microsoft Excel برای مدیریت دادهها، ایجاد جداول، فرمولنویسی و تحلیل اطلاعات.
مثال محاسبه حقوق و دستمزد یا ایجاد نمودار. - پایگاههای داده Database
استفاده از نرمافزارهای پایگاه داده مثل Microsoft Access برای ذخیره و مدیریت دادهها.
مثال ایجاد پایگاه داده مشتریان یک شرکت. - ارائه مطالب Presentation
کار با نرمافزارهایی مثل Microsoft PowerPoint برای طراحی و ارائه اسلایدهای حرفهای.
مثال ارائه گزارشها و پروژهها. - اطلاعات و ارتباطات Information and Communication
استفاده از اینترنت، ایمیل، و ابزارهای ارتباطی آنلاین برای جستجو، ارسال و دریافت اطلاعات.
مثال جستجوی گوگل، ارسال ایمیل، کار با مرورگرها.
مزایای یادگیری ICDL
- ارتقای مهارتهای کامپیوتری یادگیری پایهای و کاربردی برای کار با کامپیوتر.
- افزایش فرصتهای شغلی شرط ورود به بسیاری از مشاغل در دنیای دیجیتال.
- بهبود بهرهوری آشنایی با ابزارهایی که زندگی شخصی و حرفهای را آسانتر میکنند.
مفاهیم اساسی در حوزه فناوری اطلاعات و ارتباطات
- IT فناوری اطلاعات – Information Technology
استفاده از رایانهها، شبکهها، سختافزار و نرمافزار برای ذخیرهسازی، مدیریت و انتقال دادهها.
مثال مدیریت پایگاه داده، توسعه نرمافزار، شبکههای کامپیوتری. - ICT فناوری اطلاعات و ارتباطات – Information and Communication Technology
ترکیبی از فناوری اطلاعات IT و ابزارهای ارتباطی برای انتقال و پردازش اطلاعات، شامل اینترنت، تلفن همراه، و رسانههای دیجیتال.
مثال آموزش از راه دور، کنفرانسهای ویدیویی. - IS سیستمهای اطلاعاتی – Information Systems
ترکیب انسانها، سختافزار، نرمافزار، و دادهها برای جمعآوری، پردازش، ذخیره و توزیع اطلاعات.
مثال سیستمهای مدیریت منابع انسانی HRMS، سیستمهای حسابداری. - IoT اینترنت اشیاء – Internet of Things
شبکهای از دستگاههای فیزیکی متصل به اینترنت که اطلاعات را جمعآوری و به اشتراک میگذارند.
مثال خانههای هوشمند، دستیارهای صوتی مثل Alexa - AI هوش مصنوعی – Artificial Intelligence
شبیهسازی هوش انسانی در ماشینها برای انجام کارهایی مثل یادگیری، تصمیمگیری و حل مسئله.
مثال چتباتها، تشخیص چهره. - Big Data کلان دادهها
مجموعههای عظیم داده که بهصورت ساختاریافته یا غیرساختاریافته هستند و برای تحلیل، تصمیمگیری، و کشف الگوها استفاده میشوند.
مثال تحلیل رفتار کاربران در شبکههای اجتماعی. - Cloud Computing رایانش ابری
ارائه خدمات ذخیرهسازی و پردازش دادهها از طریق اینترنت به جای استفاده از سختافزار محلی.
مثال Google Drive، Amazon Web Services AWS - Cybersecurity امنیت سایبری
حفاظت از سیستمها و دادهها در برابر حملات سایبری.
مثال فایروالها، رمزگذاری اطلاعات. - 5G
نسل پنجم شبکههای ارتباطی که سرعت و کیفیت انتقال دادهها را بسیار افزایش میدهد.
مثال اینترنت فوق سریع برای خودروهای خودران. - Blockchain بلاکچین
فناوری دفتر کل توزیعشده برای ثبت تراکنشها بهصورت شفاف و امن.
مثال بیتکوین، قراردادهای هوشمند.
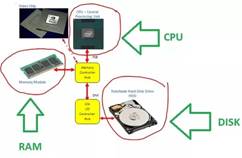
سختافزار Hardware
استارت Power Button دکمهای برای روشن و خاموش کردن دستگاه.
- بایوس BIOS نرمافزار پایه در چیپ مادربورد که راهاندازی اولیه سختافزار را انجام میدهد.
- رام ROM حافظه فقط خواندنی که اطلاعات دائمی سیستم را نگه میدارد.
- رم RAM حافظه موقت که برای پردازش سریع دادهها استفاده میشود.
- مادربورد Motherboard برد اصلی که تمام قطعات کامپیوتر را به هم متصل میکند.
- پردازنده CPU واحد پردازش مرکزی که عملیات محاسباتی را انجام میدهد.
- کارت گرافیک GPU قطعهای برای پردازش تصاویر و گرافیک.
- هارد دیسک HDD حافظهای برای ذخیرهسازی دادههای دائمی.
- درایو حالت جامد SSD حافظه سریع برای ذخیرهسازی داده.
- منبع تغذیه Power Supply قطعهای برای تأمین برق سایر قطعات.
نرمافزار Software
- سیستمعامل Operating System نرمافزاری که مدیریت سختافزار و اجرای برنامهها را بر عهده دارد.
- درایور Driver نرمافزار واسط بین سیستمعامل و سختافزار.
- برنامه Application نرمافزار برای انجام وظایف خاص مثل ویرایش متن یا بازی.
- واسط کاربری UI نمای گرافیکی یا متنی برای تعامل کاربر با سیستم.
- کد منبع Source Code دستورالعملهای نوشتهشده توسط برنامهنویس برای ایجاد نرمافزار.
- پایگاهداده Database نرمافزاری برای ذخیره و مدیریت دادهها.
تعاریف مرتبط با پردازندهها و واحد گرافیکی
شرکتها و فناوریهای مرتبط
- اینتل Intel یکی از بزرگترین تولیدکنندگان پردازندههای کامپیوتری در جهان که به طراحی و تولید پردازندههایی با کارایی بالا مثل Core i3، i5، i7 و i9 شناخته میشود.
- ایامدی AMD شرکت پیشرو دیگر در زمینه تولید پردازندهها و کارتهای گرافیکی که رقیب اصلی اینتل و انویدیا است. پردازندههای سری Ryzen از محصولات محبوب این شرکت هستند.
رَیزن Ryzen خانوادهای از پردازندههای AMD که برای کاربران عادی و حرفهای طراحی شدهاند. سری Ryzen در دستههای متنوعی مثل Ryzen 3، Ryzen 5، Ryzen 7 و Ryzen 9 عرضه میشود و به قدرت پردازش بالا و قیمت رقابتی معروف است.
پردازنده CPU
- پردازنده Processor واحد پردازش مرکزی CPU که تمامی عملیات محاسباتی و منطقی را انجام میدهد. برندهای معروف شامل Intel و AMD هستند.
- نسل Generation نشاندهنده نسل پردازنده است که تکنولوژی، معماری و عملکرد آن را مشخص میکند. مثلاً در پردازندههای اینتل، نسل 12 و 13 مثل Core i7-13700K بهبودهایی در سرعت و مصرف انرژی دارند.
کارت گرافیک GPU
- کارت گرافیک GPU واحد پردازش گرافیکی برای پردازش تصاویر، ویدئوها و اجرای بازیها. کارت گرافیکها یا مستقل هستند مانند NVIDIA GeForce یا AMD Radeon یا به صورت مجتمع با CPU عرضه میشوند مثل Intel UHD Graphics.
- انویدیا NVIDIA شرکت پیشرو در طراحی کارتهای گرافیکی مستقل با سریهای معروف مثل RTX و GTX.
- کارت مجتمع Integrated GPU گرافیک داخلی که در CPU تعبیه شده و برای کارهای سبک استفاده میشود. مثلاً Intel UHD یا AMD Radeon Vega.
- کارت مستقل Dedicated GPU کارتهای گرافیکی قدرتمند که به صورت جداگانه به مادربورد وصل میشوند و برای بازی، رندرینگ و هوش مصنوعی استفاده میشوند.
معماری و نسلها
- معماری Architecture طراحی پایه سختافزار CPU یا GPU که مشخص میکند یک محصول چقدر بهینه و سریع است. مثلاً معماری Zen در پردازندههای Ryzen یا Alder Lake در نسل 12 اینتل.
- واحدهای پردازشی Cores تعداد هستههای موجود در CPU که هرکدام میتوانند عملیات مجزا انجام دهند. تعداد بیشتر هستهها به معنی قابلیت پردازش بیشتر به صورت همزمان است.
- فرکانس Clock Speed سرعت پردازش پردازنده که بر حسب گیگاهرتز GHz اندازهگیری میشود. فرکانس بالاتر معمولاً به معنای سرعت بیشتر است.
آزمون عملی Word و مرورآزمون عملی Word و مرور
آموزشگاه هوش مصنوعی
1- ایجاد یک سند جدید
یک سند جدید باز کرده و نام آن را به tirotir1.docx ذخیره کنید.
2- تنظیمات فونت
متنی را تایپ کنید و سپس فونت آن را به B Nazanin تغییر داده و اندازه را روی ۱۴ تنظیم کنید.
3- اعمال سبک (Styles)
عنوانی بنویسید و از استایل Heading 1 برای آن استفاده کنید.
4- تراز بندی متن
متنی را در وسط (Center) و متنی دیگر را در راست (Right) تراز کنید.
5- ایجاد لیست شمارهای
یک لیست شمارهای با ۵ آیتم ایجاد کنید، مثل:
- نام
- نام خانوادگی
- شماره تماس
6- ایجاد لیست بولتدار (Bulleted List)
یک لیست بولتدار برای اقلام خرید بنویسید، مثل:
- نان
- شیر
- تخممرغ
7- تنظیم فاصله خطوط (Line Spacing)
فاصله خطوط را برای یک پاراگراف روی ۱.۵ تنظیم کنید.
8- اضافه کردن تصویر
یک تصویر دلخواه را به سند وارد کرده و اندازه آن را تغییر دهید.
9- ایجاد جدول ساده
یک جدول ۳ در ۵ برای ثبت اطلاعات (نام، سن، شماره تماس) ایجاد کنید.
10- اضافه کردن حاشیه به صفحه (Page Borders)
به سند خود یک حاشیه ساده اضافه کنید.
11- تنظیم سرصفحه و پاصفحه (Header and Footer)
در سرصفحه، نام سند را تایپ کنید و در پاصفحه شماره صفحه اضافه کنید.
12- ایجاد یک متن با رنگ سفارشی
متنی تایپ کنید و رنگ آن را به آبی تغییر دهید.
13- استفاده از Bold، Italic، Underline
یک متن کوتاه تایپ کنید و سپس آن را بولد، ایتالیک و زیرخطدار کنید.
14- ایجاد لینک (Hyperlink)
یک لینک به آدرس وبسایت مانندGoogle اضافه کنید.
15- استفاده از Find and Replace
کلمهای را در متن پیدا کنید و آن را با یک کلمه دیگر جایگزین کنید.
16- افزودن شماره صفحه (Page Numbers)
شماره صفحه را در پایین سمت راست اضافه کنید.
17- ایجاد پاورقی (Footnote)
یک پاورقی برای توضیح یک کلمه در متن اضافه کنید.
18- تنظیم جهت صفحه (Page Orientation)
جهت صفحه را به افقی (Landscape) تغییر دهید.
19- استفاده از SmartArt
یک نمودار سازمانی ساده با استفاده از SmartArt ایجاد کنید.
20- ذخیره سند در فرمت PDF
سند را با فرمت PDF ذخیره کنید.
موارد دیگر:
- اضافه کردن Watermark
- استفاده از Columns برای متن چند ستونه.
- تنظیم Margins
- افزودن Bookmark به متن.
- استفاده از Cover Page
- استفاده از Text Box برای ایجاد متن شناور.
- تنظیم خودکار شماره تیترها با استفاده از Multilevel List
- اضافه کردن Symbol مانند علامت درج شده در اسناد رسمی
- کار با Review برای نظرات و ویرایش.
- انجام Page Break برای جدا کردن صفحات.
- سفارشیسازی روبان.
- فرمول در ورد:

- ایجاد یک سند جدید در Word
باز کردن Word –> انتخاب Blank Document. - ذخیره یک سند
فشردن Ctrl+S –> انتخاب مکان ذخیره –> تایپ نام فایل. - تغییر فونت متن
انتخاب متن –> انتخاب فونت دلخواه از تب Home. - تغییر اندازه فونت
انتخاب متن –> انتخاب اندازه فونت از تب Home. - استفاده از قالببندی پررنگ
انتخاب متن –> فشار دادن Ctrl+B یا کلیک روی Bold از تب Home. - استفاده از قالببندی ایتالیک
انتخاب متن –> فشار دادن Ctrl+I یا کلیک روی Italic از تب Home. - استفاده از قالببندی زیرخط
انتخاب متن –> فشار دادن Ctrl+U یا کلیک روی Underline از تب Home. - ایجاد یک لیست شمارهدار
انتخاب متن –> کلیک روی شمارهدار از تب Home. - ایجاد یک لیست نقطهدار
انتخاب متن –> کلیک روی لیست نقطهدار از تب Home. - تنظیم حاشیه سند
باز کردن تب Layout –> Margins –> انتخاب نوع حاشیه. - وارد کردن تصویر در سند
انتخاب تب Insert –> Pictures –> انتخاب تصویر از محل ذخیره. - وارد کردن جدول در سند
انتخاب تب Insert –> Table –> انتخاب تعداد ردیف و ستون. - ایجاد عنوان (Heading)
انتخاب متن –> انتخاب Heading از تب Home. - تنظیم چیدمان صفحه (Portrait/Landscape)
باز کردن تب Layout –> Orientation –> انتخاب Portrait یا Landscape. - درج شماره صفحه
باز کردن تب Insert –> Page Number –> انتخاب محل قرارگیری شماره صفحه. - استفاده از قابلیت جستجو
فشار دادن Ctrl+F –> تایپ کلمه یا عبارت مورد جستجو. - تنظیم فاصله بین خطوط
انتخاب متن –> باز کردن تب Home –> Paragraph –> تنظیم Line Spacing. - استفاده از ابزار ویرایش هجی
انتخاب تب Review –> Spelling & Grammar –> بررسی هجی. - اضافه کردن حاشیه به صفحه
باز کردن تب Design –> Page Borders –> تنظیمات حاشیه. - وارد کردن پیوند (Hyperlink)
انتخاب متن –> راستکلیک –> Hyperlink –> تایپ URL. - چاپ یک سند
فشار دادن Ctrl+P –> انتخاب پرینتر –> انتخاب تنظیمات چاپ. - تغییر رنگ متن
انتخاب متن –> انتخاب رنگ از تب Home. - استفاده از حالت نمایش Full Screen
فشار دادن Ctrl+Alt+F1 یا انتخاب View –> Full Screen Reading. - ادغام دادهها با اکسل (Mail Merge)
باز کردن تب Mailings –> Start Mail Merge –> انتخاب نوع ادغام. - وارد کردن تاریخ و زمان
انتخاب تب Insert –> Date & Time –> انتخاب فرمت تاریخ. - فعال کردن قابلیت نظردهی
انتخاب تب Review –> New Comment –> نوشتن نظر. - اعمال سبکهای مختلف به پاراگرافها
انتخاب پاراگراف –> انتخاب سبک از تب Home. - چرخاندن تصویر
انتخاب تصویر –> کلیک روی گزینه Rotate از تب Format. - نمایش خطوط راهنما
انتخاب تب View –> نمایش گزینه Ruler. - استفاده از ابزار مقایسه اسناد
انتخاب تب Review –> Compare –> انتخاب دو سند برای مقایسه. - اضافه کردن خط افقی به سند
انتخاب تب Insert –> Shapes –> انتخاب Line –> کشیدن خط افقی. - اضافه کردن شماره فصل
انتخاب تب References –> Insert Caption –> انتخاب نوع شمارهگذاری. - تنظیم جهت متن (راستچین یا چپچین)
انتخاب تب Home –> راستچین یا چپچین کردن متن از گزینه Paragraph. - استفاده از کادر متن
انتخاب تب Insert –> Text Box –> انتخاب سبک کادر متن. - قرار دادن علامت ویژه (مثل علامت ® یا ©)
انتخاب تب Insert –> Symbol –> انتخاب علامت دلخواه. - استفاده از ابزار SmartArt
انتخاب تب Insert –> SmartArt –> انتخاب نوع SmartArt. - تنظیم رنگ پسزمینه سند
انتخاب تب Design –> Page Color –> انتخاب رنگ دلخواه. - ایجاد پیوست در ایمیل از داخل ورد
انتخاب تب File –> Share –> Email –> Attach to Email. - افزودن جدول محتویات
انتخاب تب References –> Table of Contents –> انتخاب نوع جدول محتویات. - جابجایی پاراگرافها
انتخاب پاراگراف –> کشیدن با موس به محل دلخواه. - استفاده از ویژگی Track Changes
انتخاب تب Review –> Track Changes –> فعال کردن تغییرات. - گذاشتن علامت Check Box
انتخاب تب Insert –> Symbol –> انتخاب علامت Check Box. - تغییر سبک پاراگراف
انتخاب پاراگراف –> انتخاب Style از تب Home. - درج شکاف صفحه (Page Break)
فشار دادن Ctrl+Enter. - تغییر فرمت یک فایل به PDF
انتخاب تب File –> Save As –> انتخاب PDF از نوع فایل. - تنظیم پشتیبانی از زبانهای مختلف
انتخاب تب Review –> Language –> Set Proofing Language. - ویرایش تصاویر داخل سند
انتخاب تصویر –> انتخاب تب Picture Tools –> انجام ویرایش. - ایجاد فهرست منابع
انتخاب تب References –> Manage Sources –> افزودن منابع جدید. - اضافه کردن پاورقی
انتخاب تب References –> Insert Footnote. - تغییر اندازه صفحات با توجه به محتویات
انتخاب تب View –> Zoom –> انتخاب درصد مناسب. - ایجاد جدول چند ستونی
پاسخ: انتخاب تب Insert –> Table –> انتخاب تعداد ردیفها و ستونها. - اضافه کردن شماره صفحه به جدول
پاسخ: انتخاب تب Insert –> Page Number –> انتخاب محل قرارگیری شماره صفحه. - ایجاد کادر برای صفحه
پاسخ: انتخاب تب Design –> Page Borders –> انتخاب نوع و تنظیمات کادر. - تنظیم قاب برای متن
پاسخ: انتخاب متن –> راستکلیک –> Borders and Shading –> انتخاب نوع قاب. - تنظیم متن به حالت شفاف (Transparent)
پاسخ: انتخاب متن –> انتخاب تب Home –> در قسمت Font –> تنظیم Transparency از ویژگیهای رنگ. - تغییر رنگ پسزمینه برای سلولهای جدول
پاسخ: انتخاب سلولهای جدول –> انتخاب تب Design –> Shading –> انتخاب رنگ. - وارد کردن تصویر به داخل یک سلول جدول
پاسخ: انتخاب سلول جدول –> انتخاب تب Insert –> Pictures –> انتخاب تصویر. - افزودن سایه به متن
پاسخ: انتخاب متن –> انتخاب تب Home –> Effects –> Shadow. - ترتیب و مرتبسازی دادهها در جدول
پاسخ: انتخاب جدول –> انتخاب تب Layout –> Sort –> تنظیم ترتیب دادهها. - چند خط کردن متن در یک سلول جدول
پاسخ: انتخاب سلول جدول –> راستکلیک –> Format Cells –> انتخاب گزینه Wrap Text. - چرخاندن متن در جدول
پاسخ: انتخاب سلول جدول –> راستکلیک –> Text Direction –> انتخاب جهت متن. - اضافه کردن مرز به سلولها در جدول
پاسخ: انتخاب سلولها –> انتخاب تب Design –> Borders –> انتخاب نوع مرز. - تنظیم فاصله بین سلولهای جدول
پاسخ: انتخاب جدول –> راستکلیک –> Table Properties –> Cell –> انتخاب Padding. - درج جدول به صورت متنی
پاسخ: انتخاب تب Insert –> Table –> انتخاب Table of Text –> وارد کردن متن. - تنظیم عرض ستونها و ارتفاع ردیفها در جدول
پاسخ: انتخاب جدول –> راستکلیک –> Table Properties –> تنظیم اندازه ستونها و ردیفها. - قرار دادن تصویر به عنوان پسزمینه در جدول
پاسخ: انتخاب سلولهای جدول –> راستکلیک –> Table Properties –> Fill –> انتخاب تصویر. - استفاده از فونتهای مختلف در داخل یک جدول
پاسخ: انتخاب متن داخل سلولها –> انتخاب فونت از تب Home. - تنظیم صفحه به صورت چند ستونه
پاسخ: انتخاب تب Layout –> Columns –> انتخاب تعداد ستونها. - اضافه کردن حاشیه برای صفحه در Word
پاسخ: انتخاب تب Design –> Page Borders –> انتخاب نوع حاشیه. - افزودن شمارهگذاری سفارشی در داخل جدول
پاسخ: انتخاب تب Insert –> Quick Parts –> Field –> انتخاب گزینه شمارهگذاری.
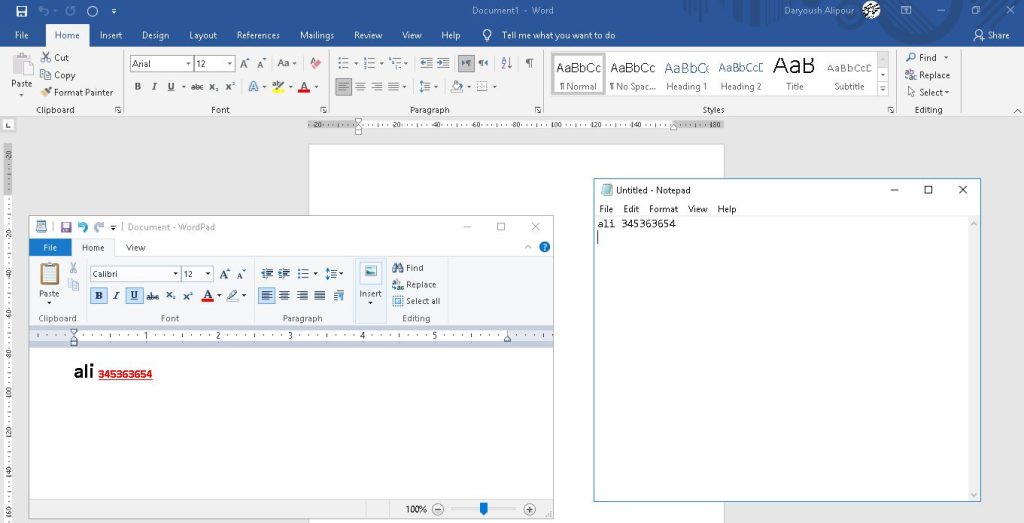
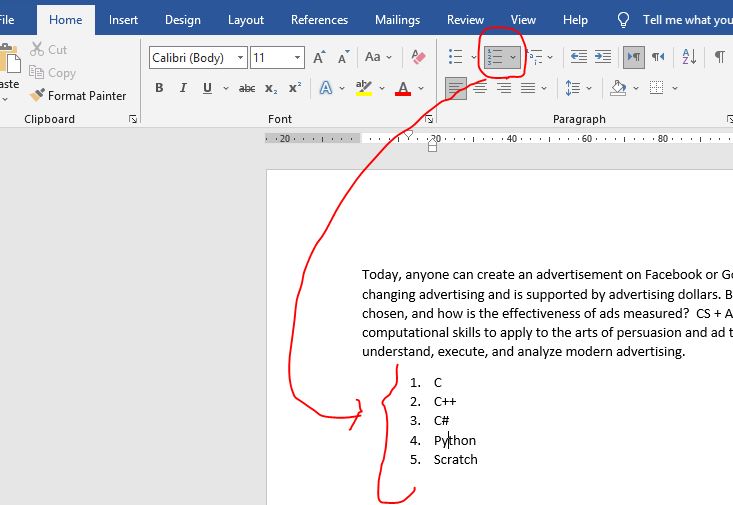
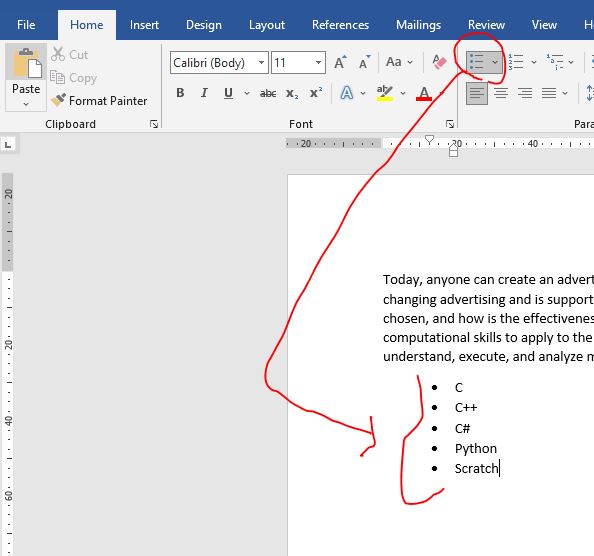
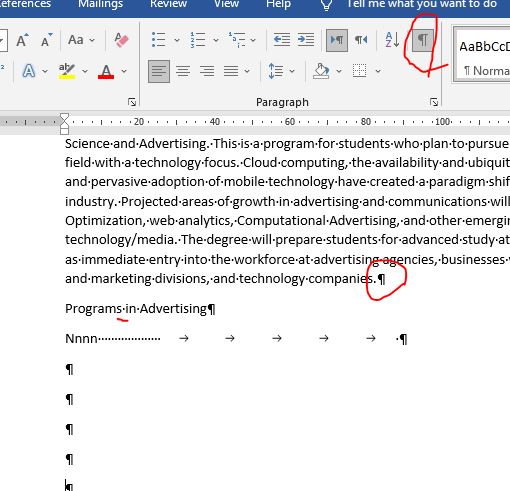
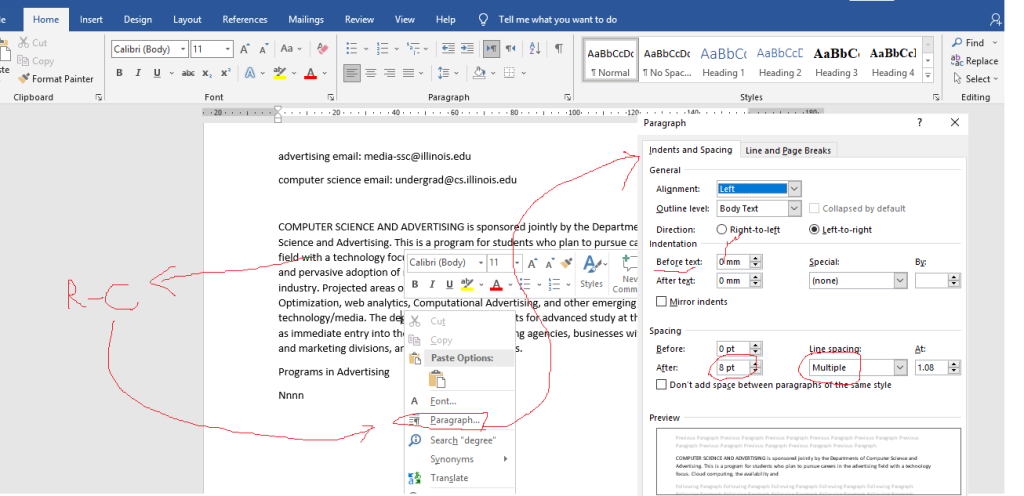
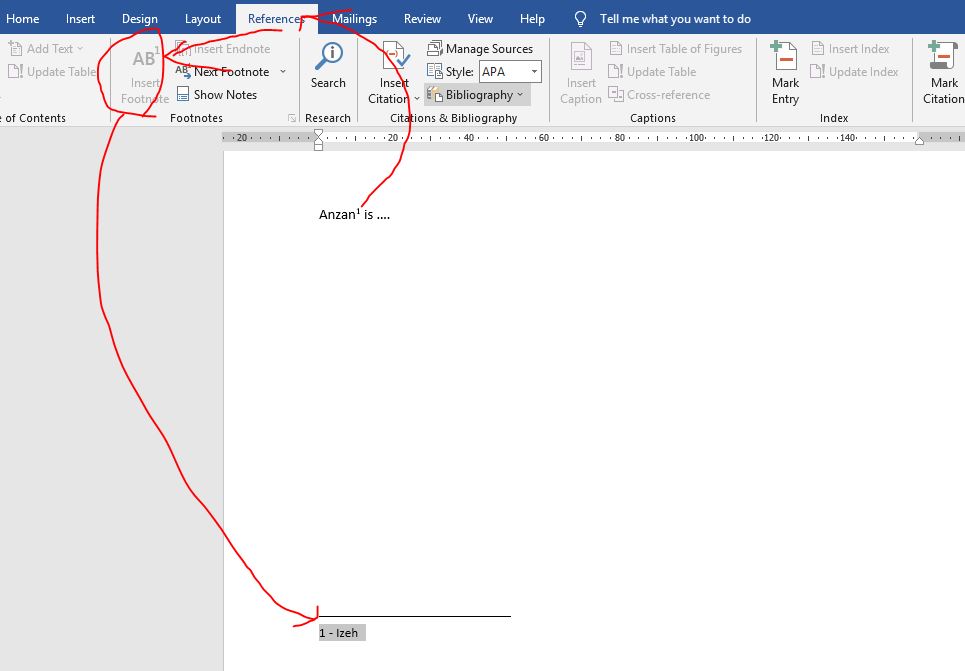
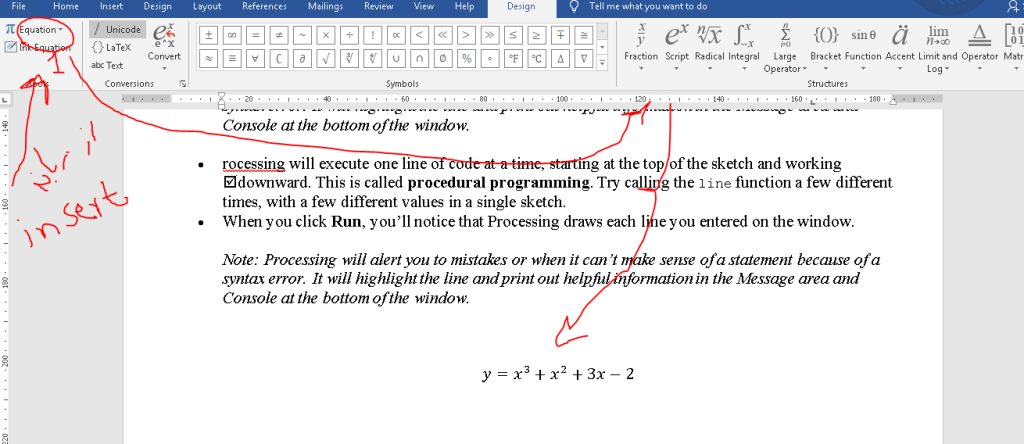
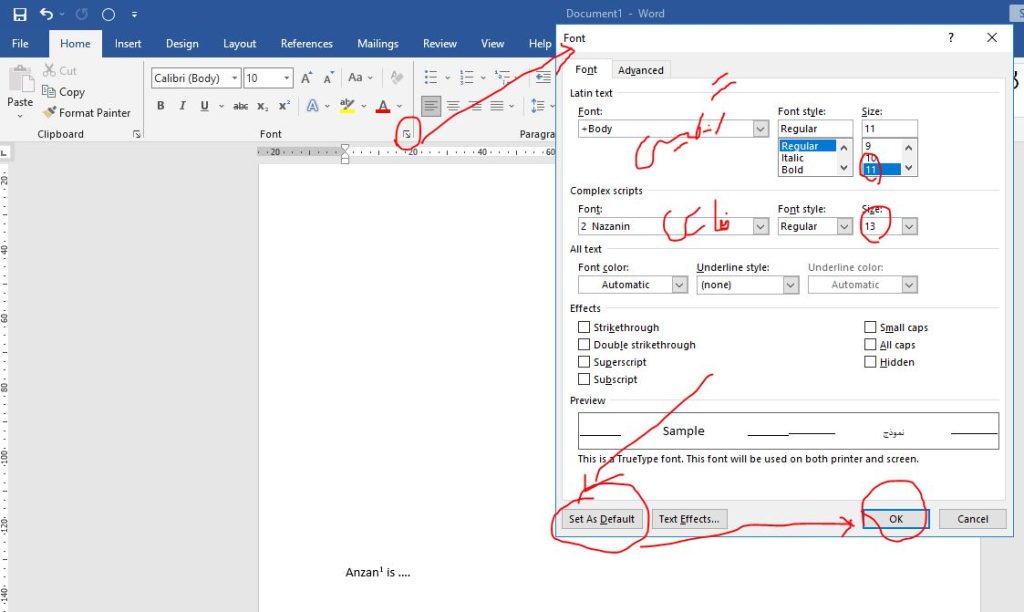
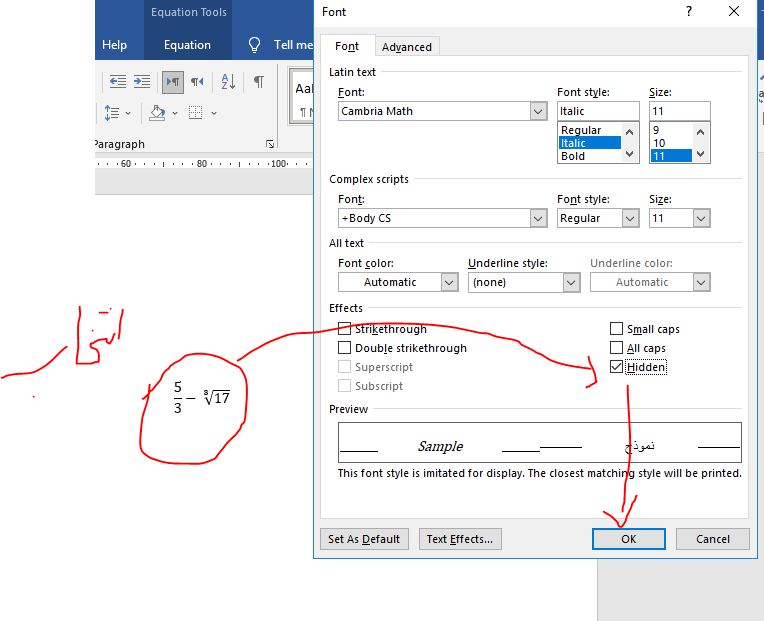
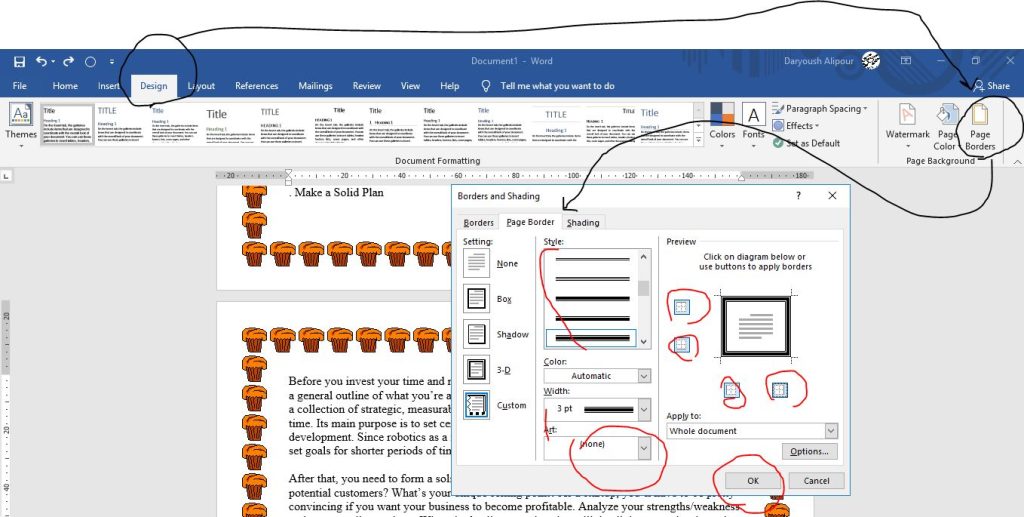
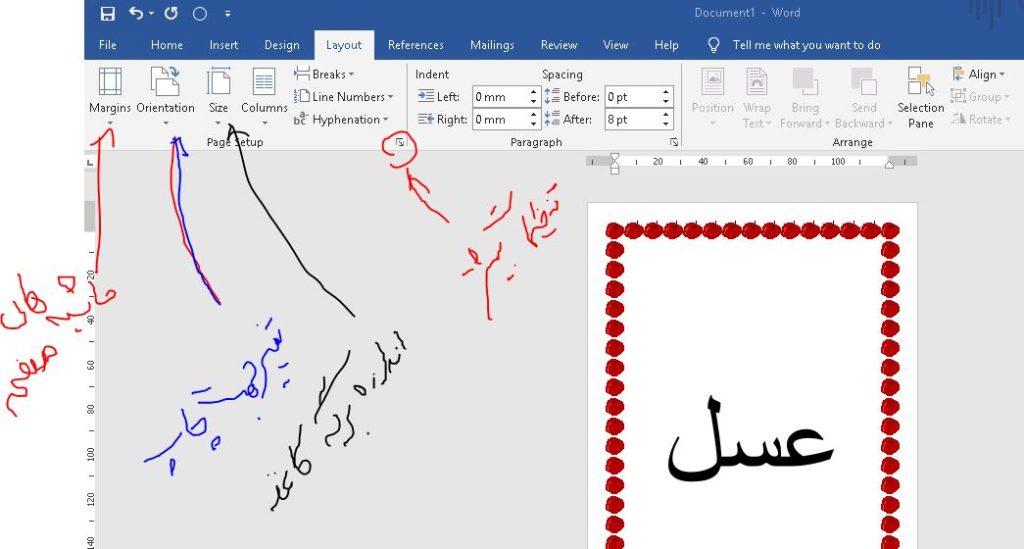
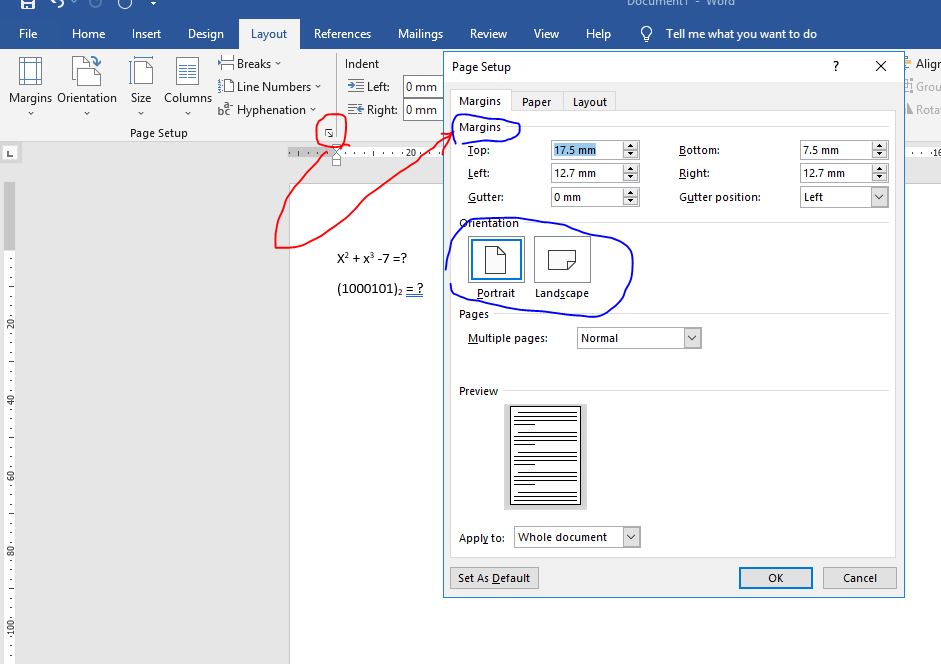
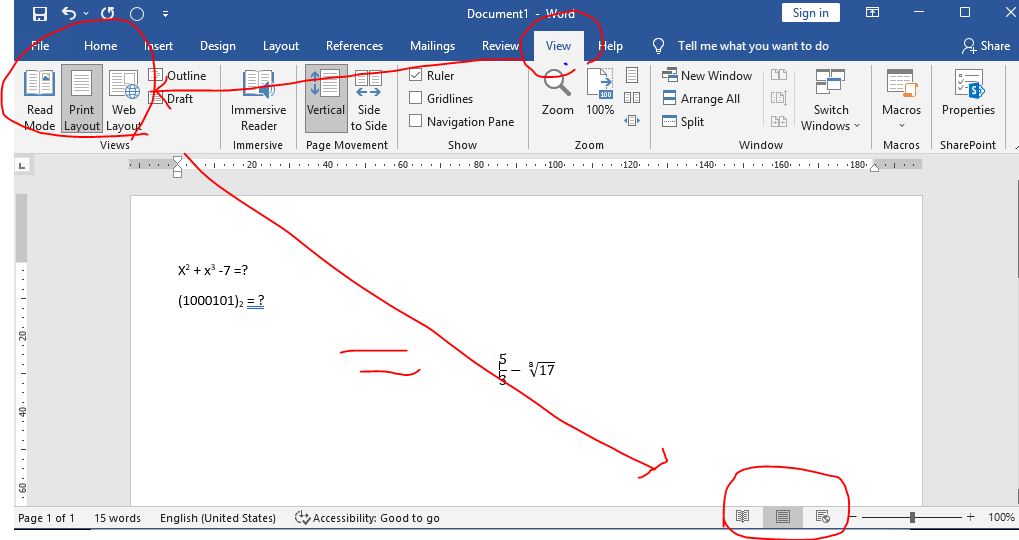
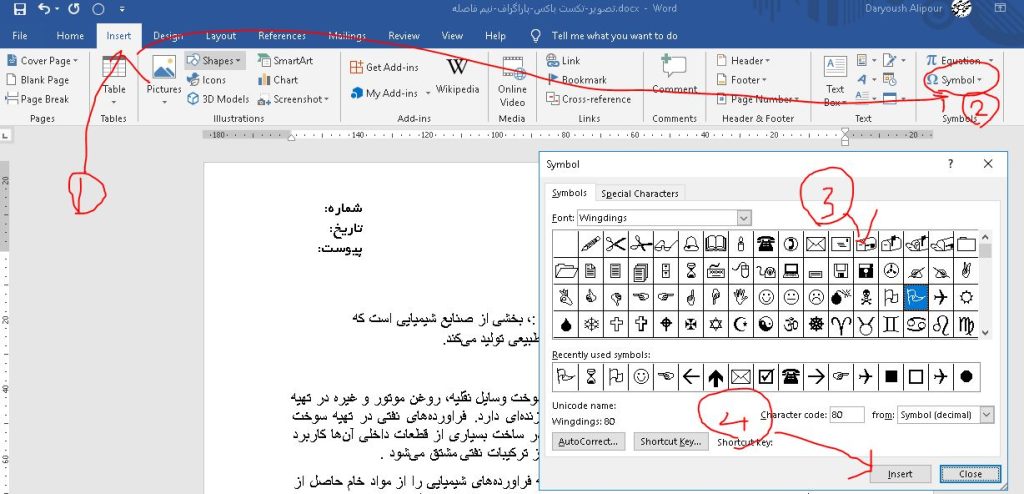
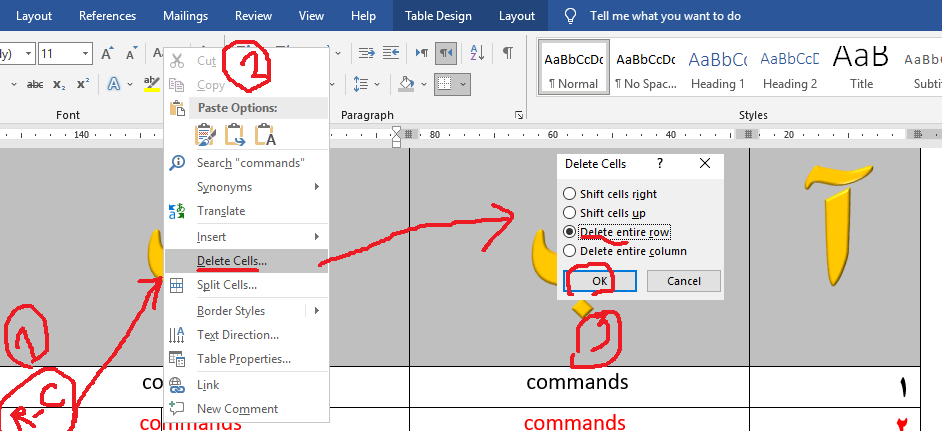
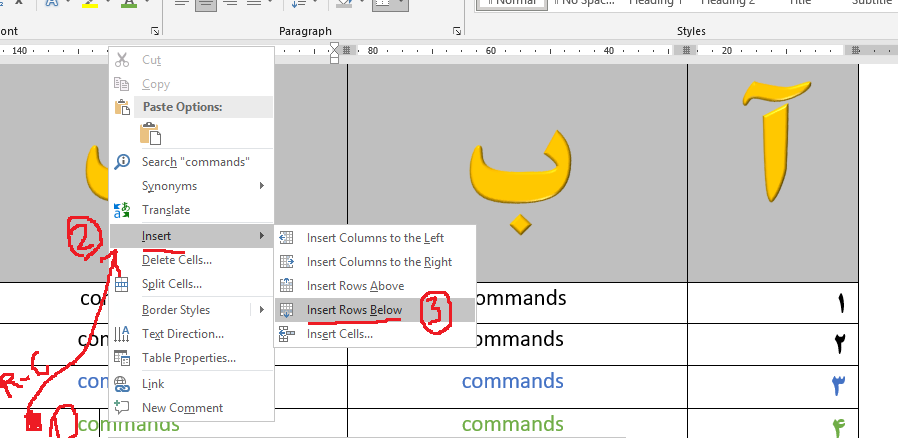
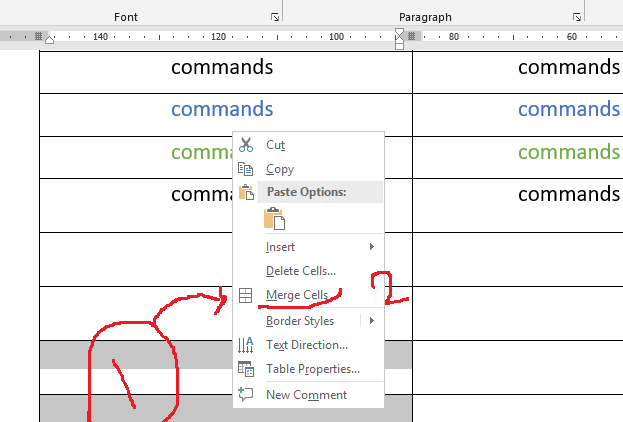
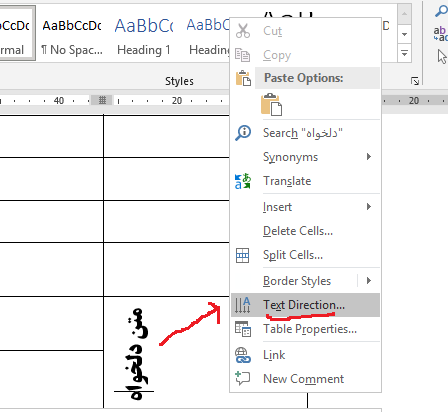
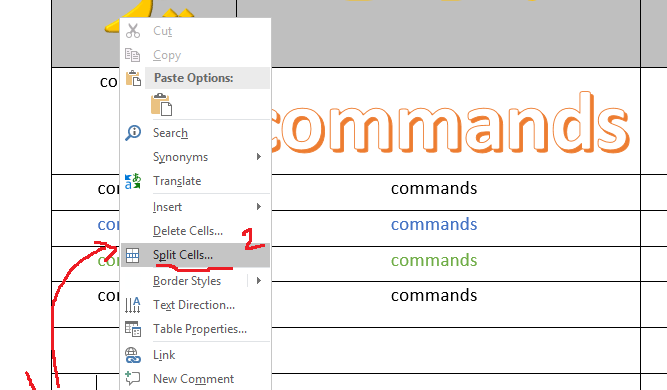
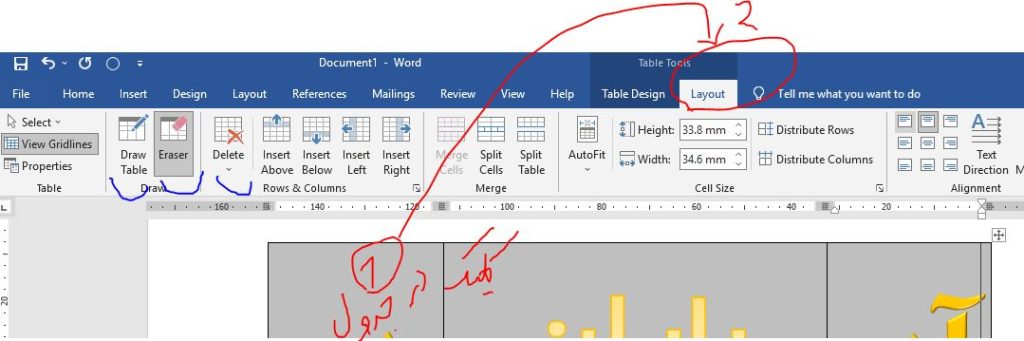
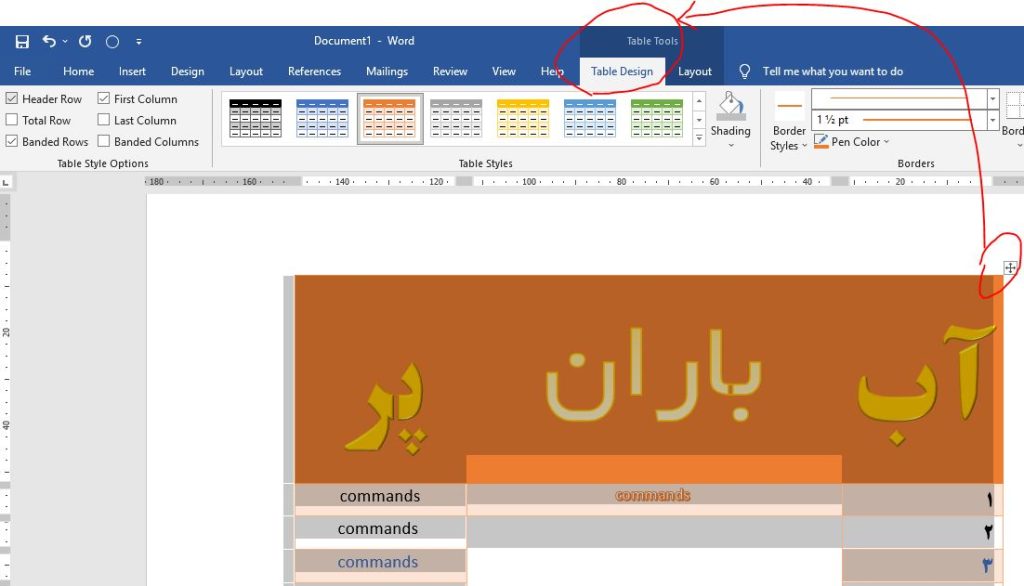
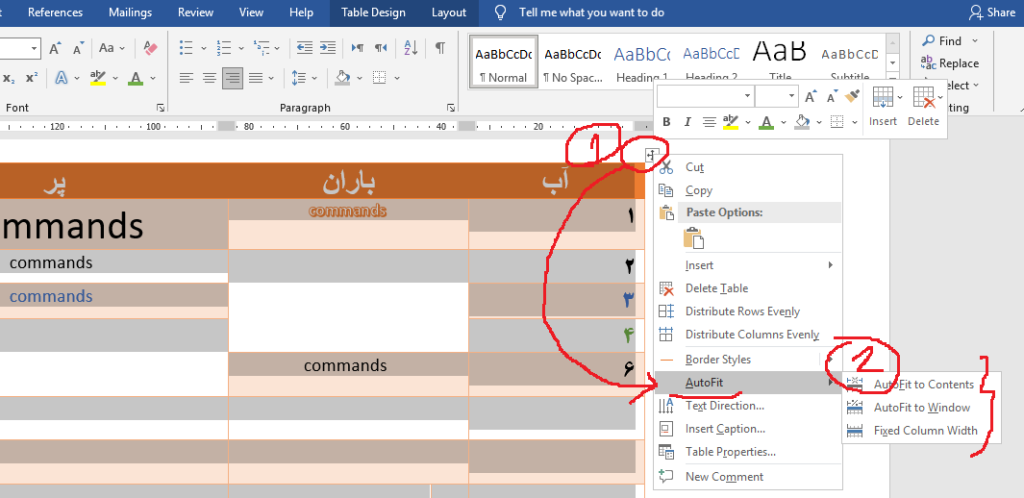
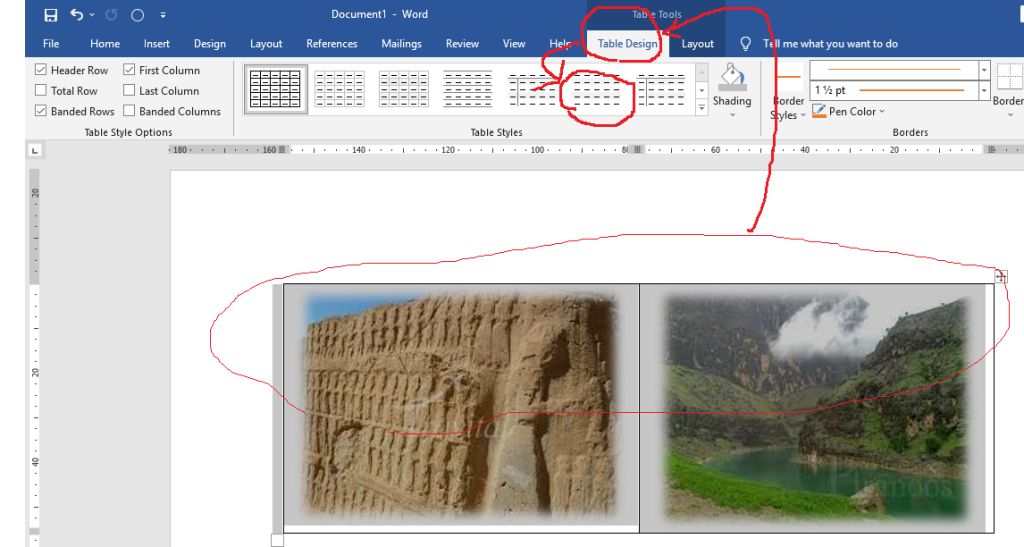
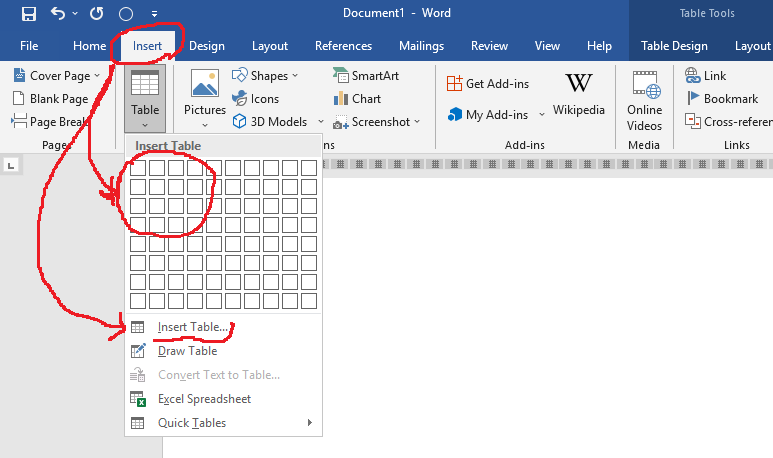
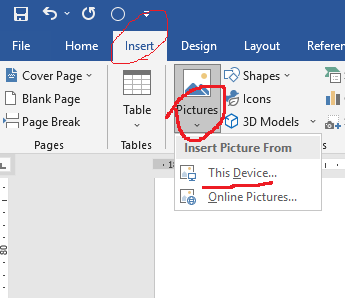
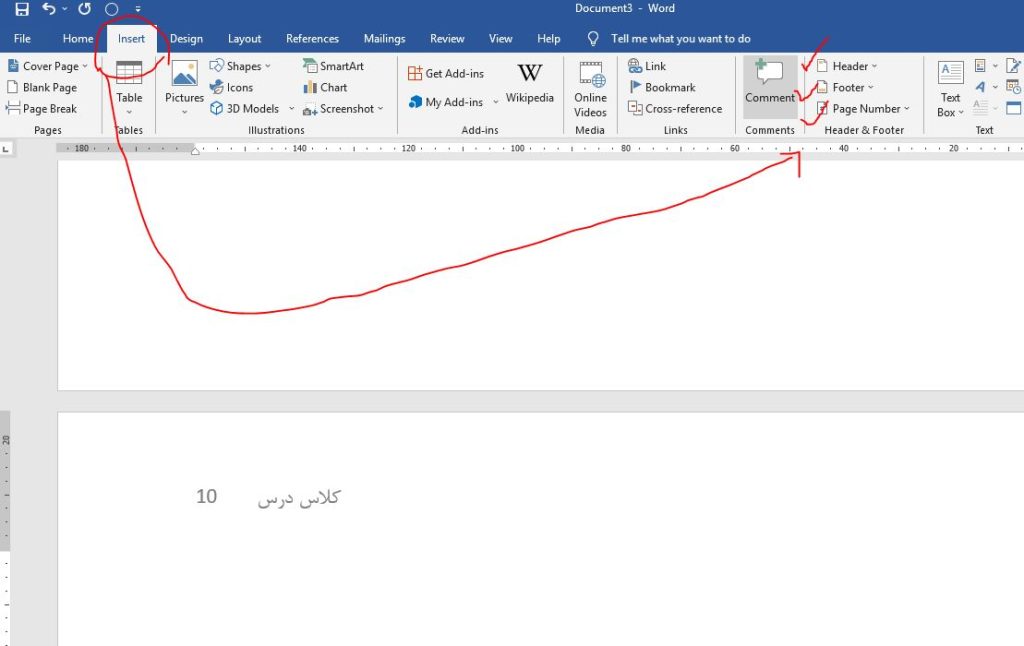
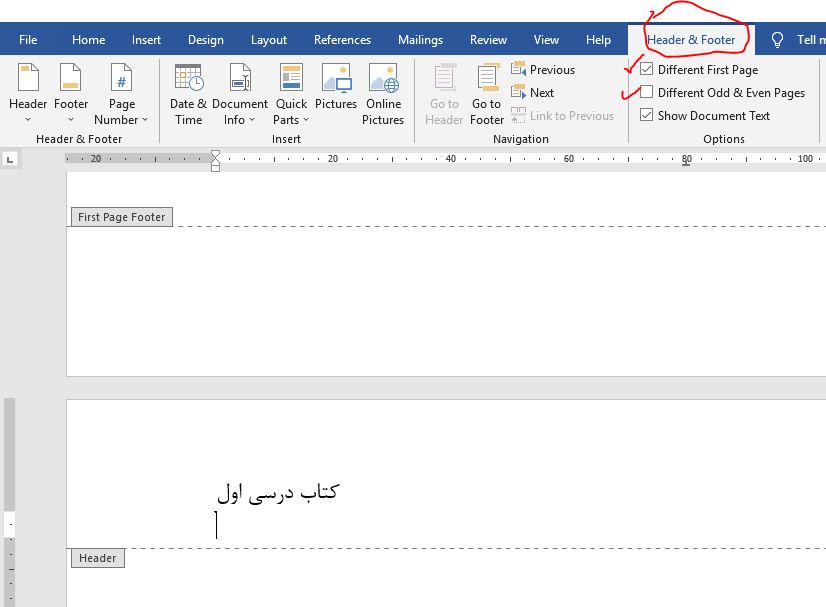
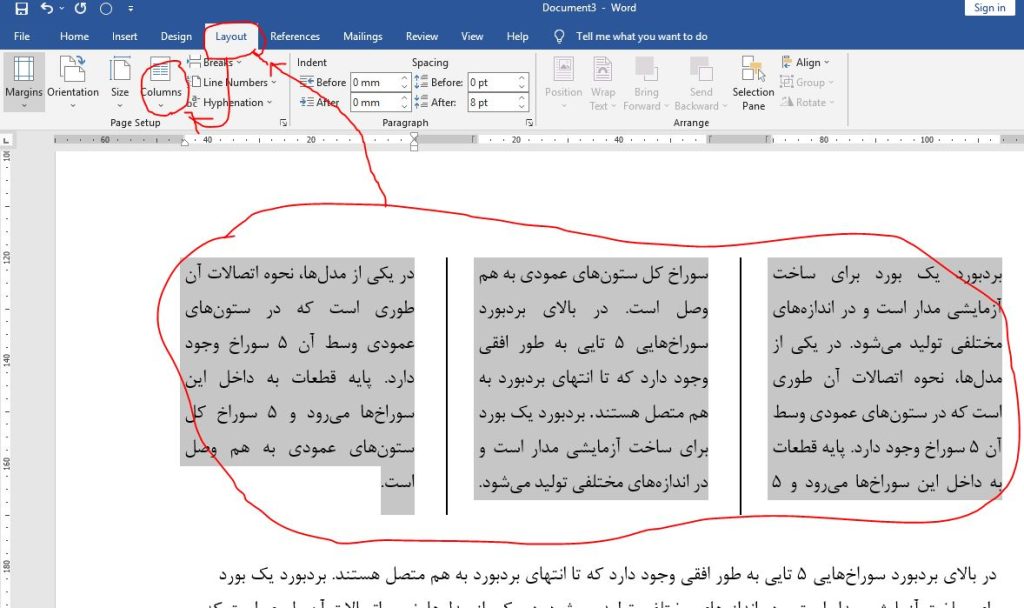
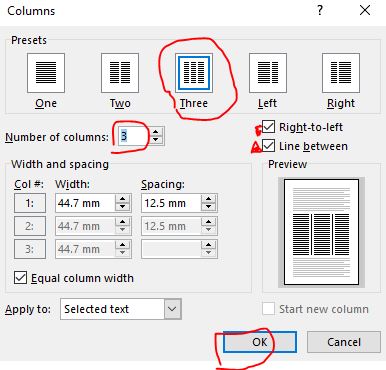
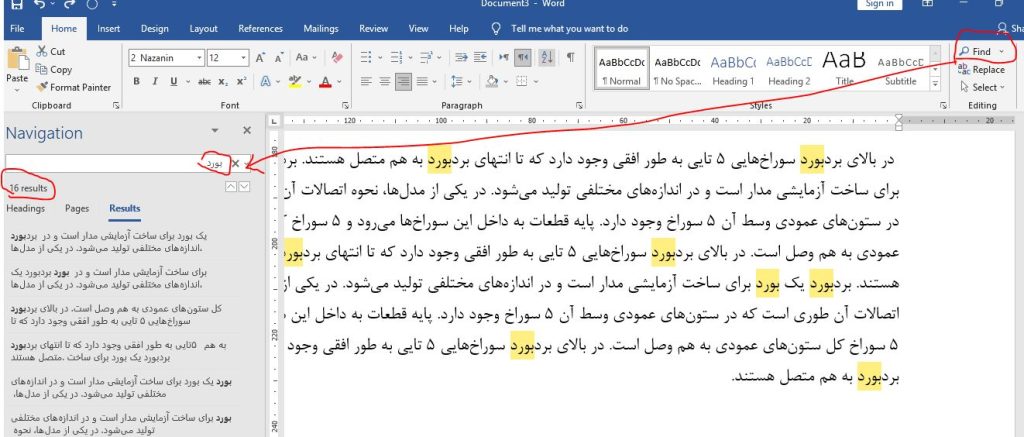
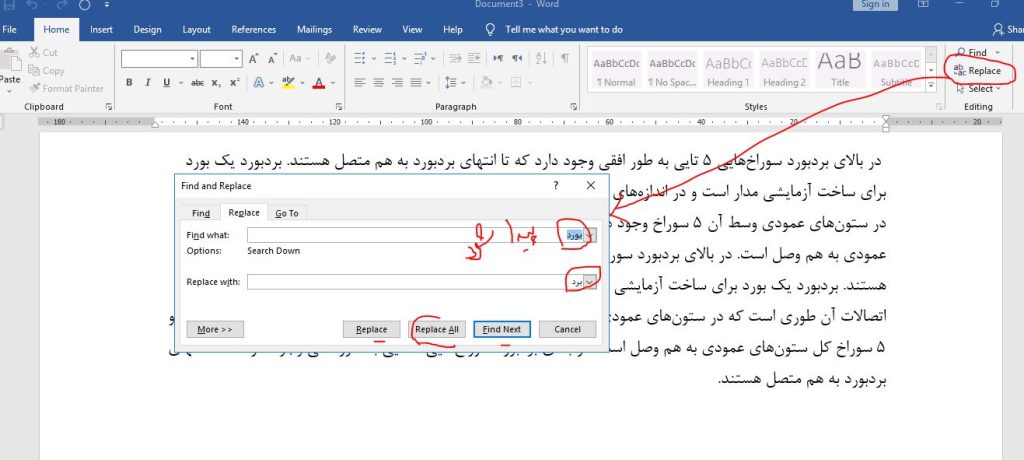
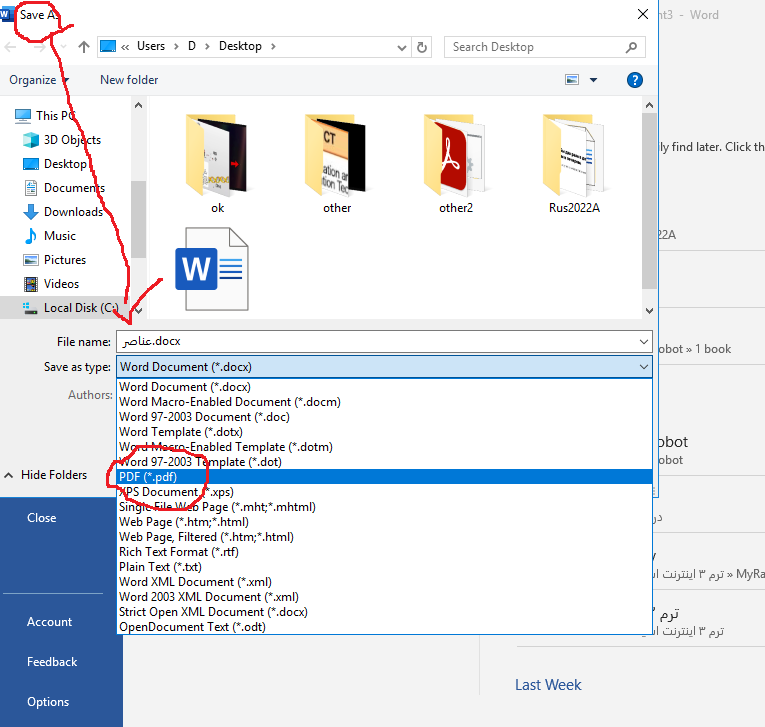
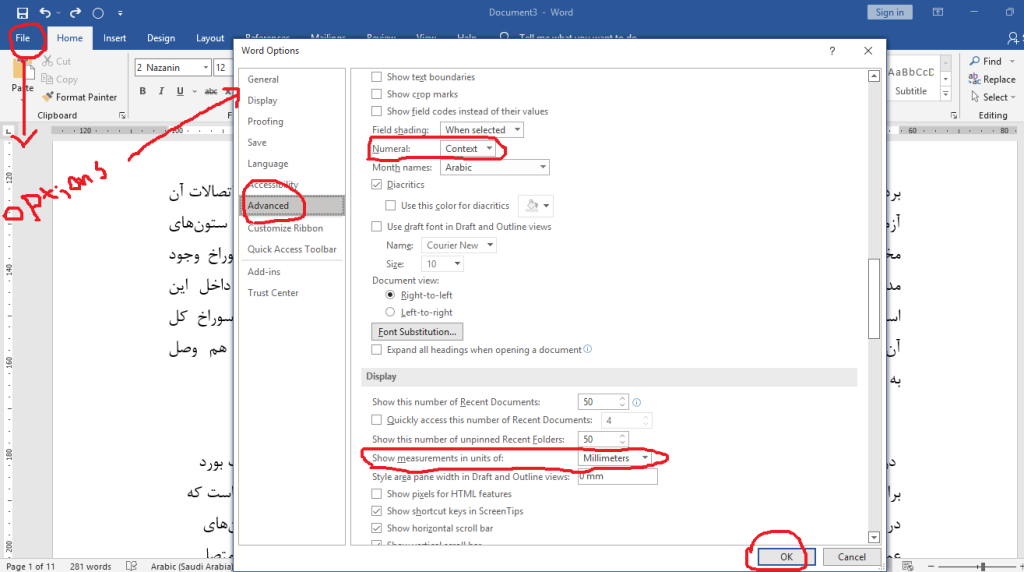
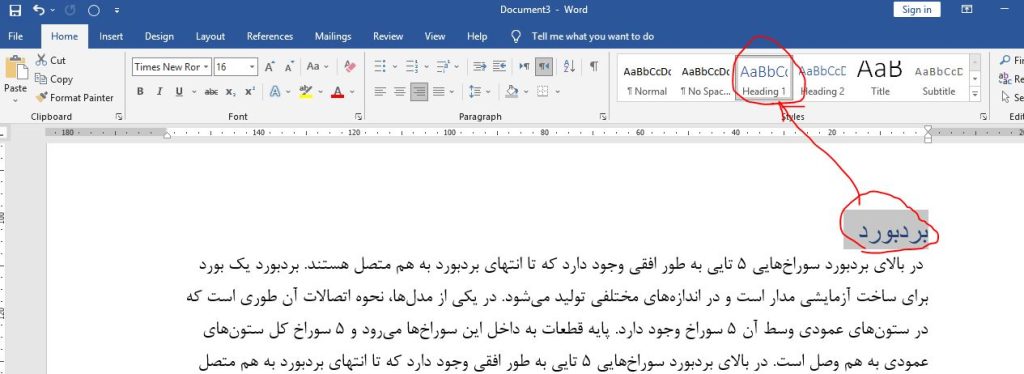
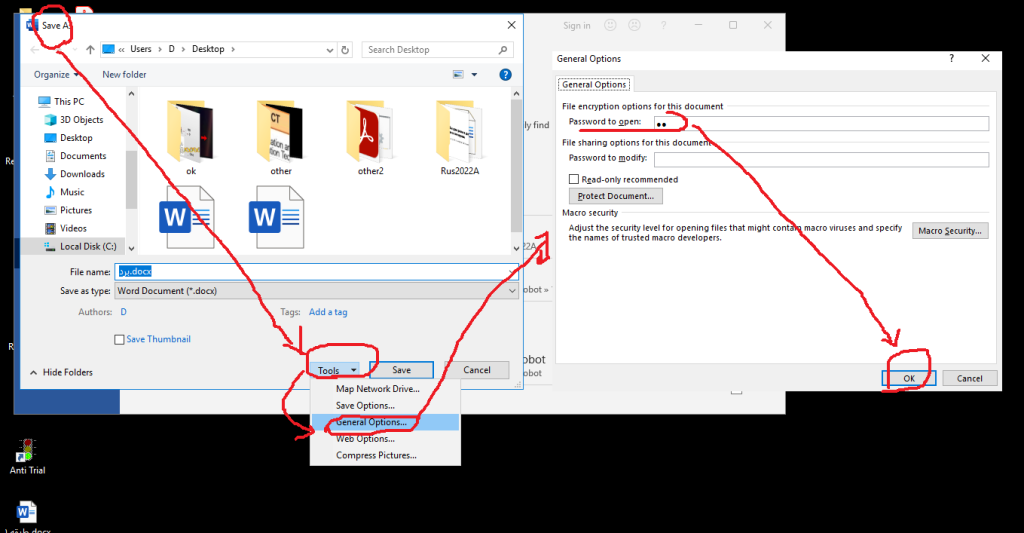
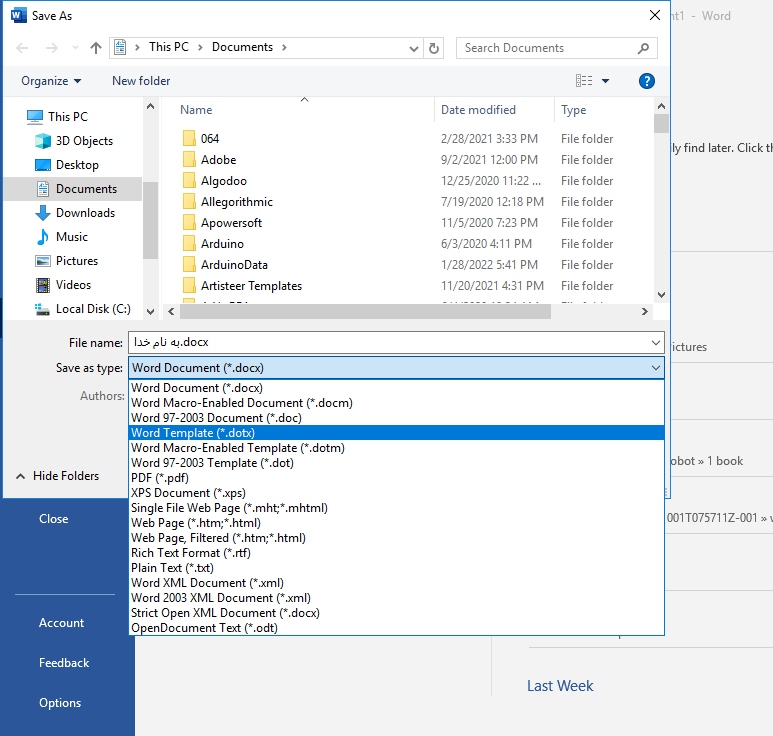
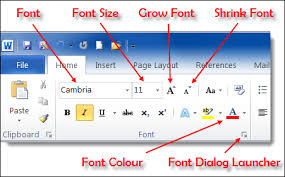
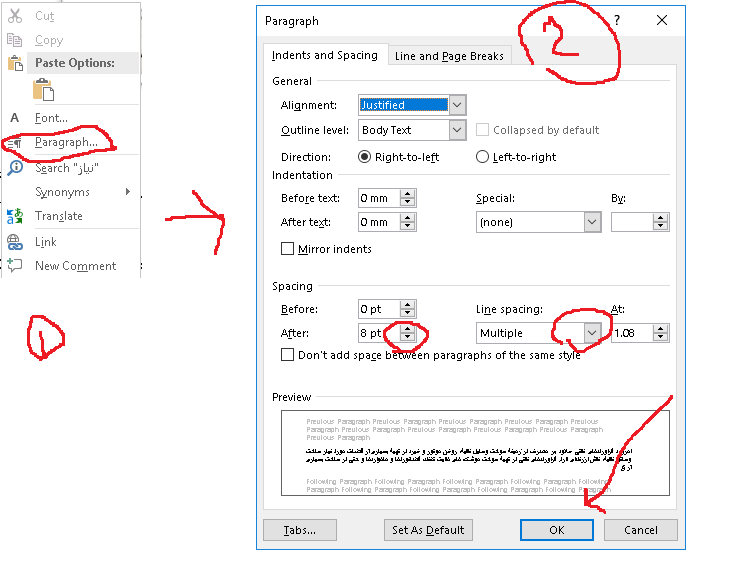

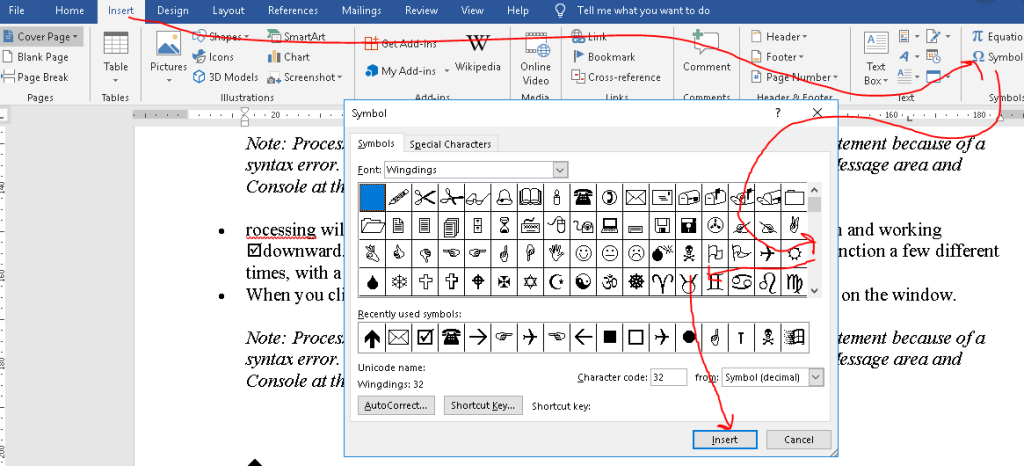
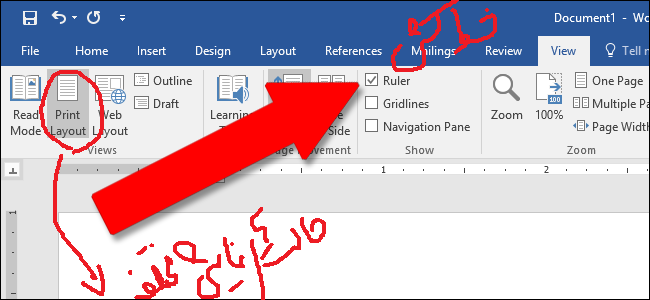
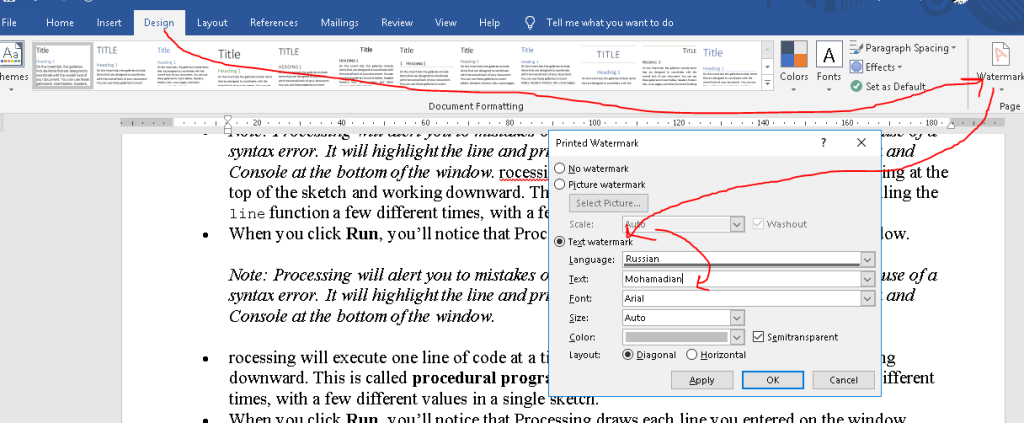
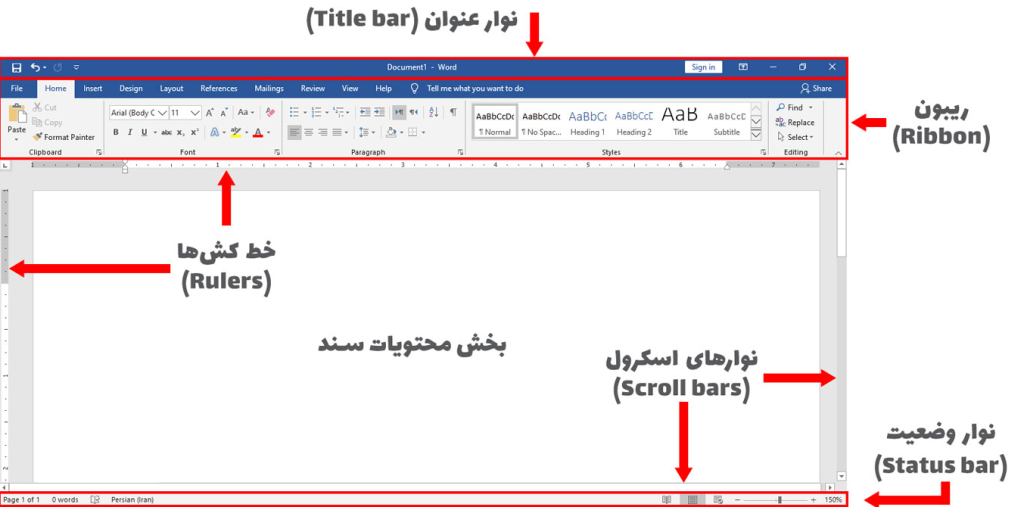
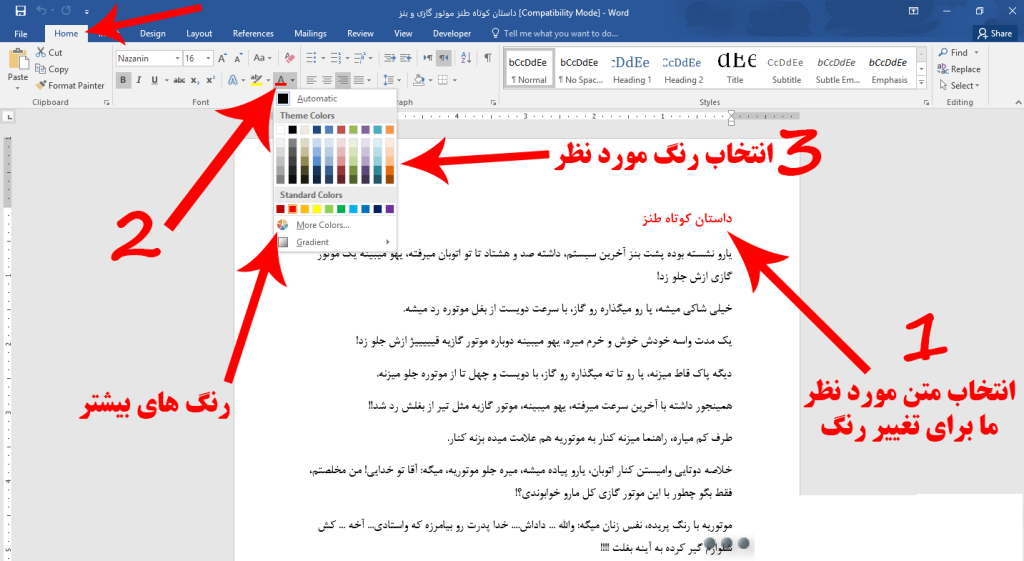
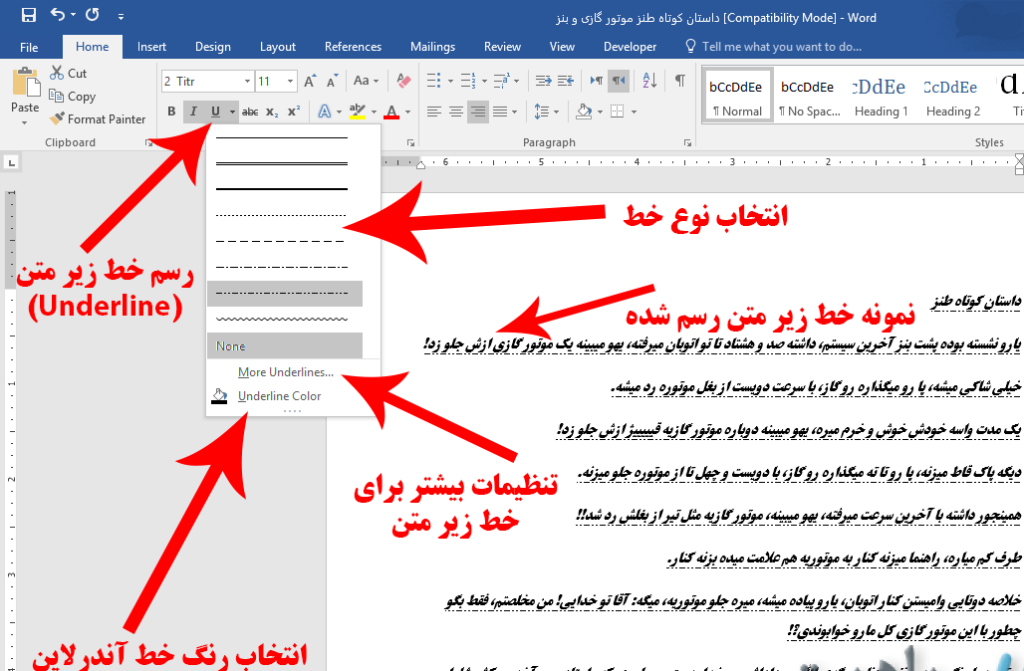
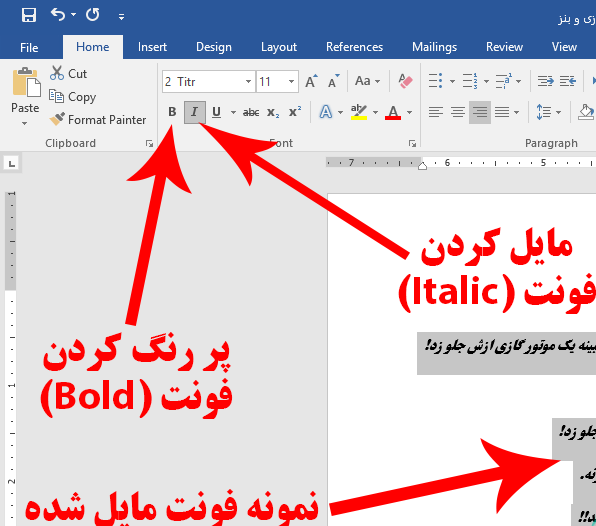
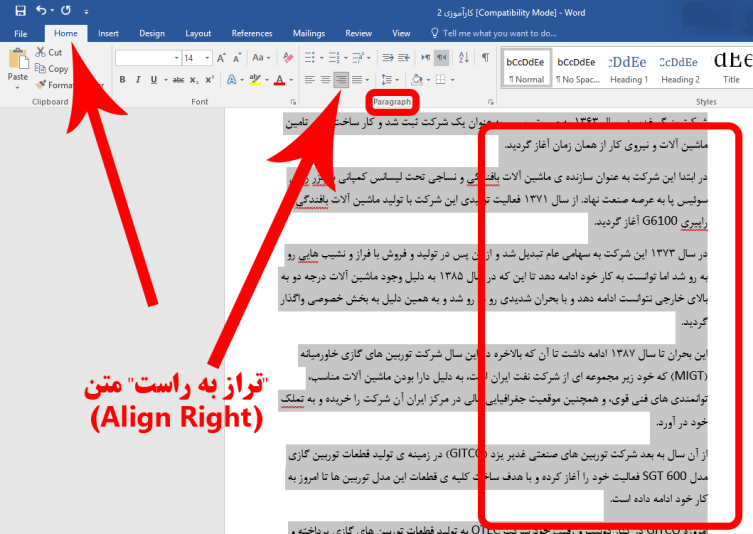
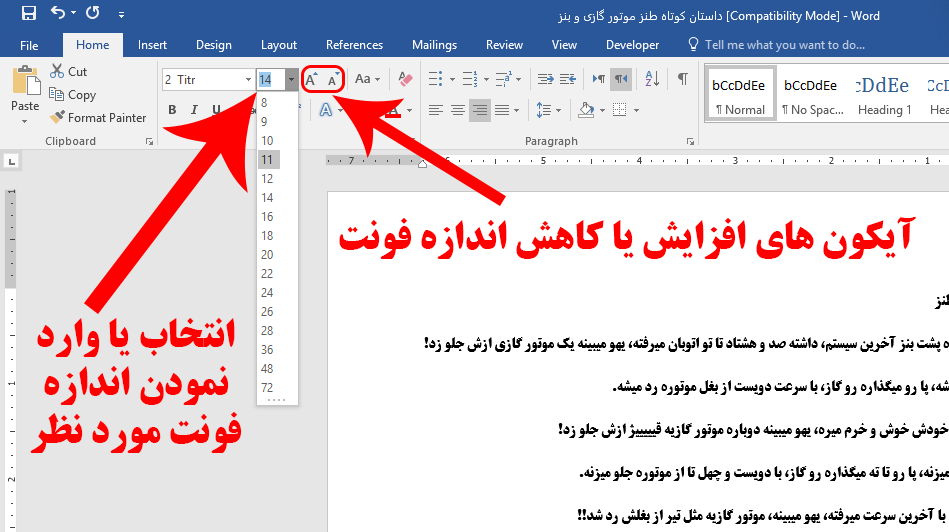
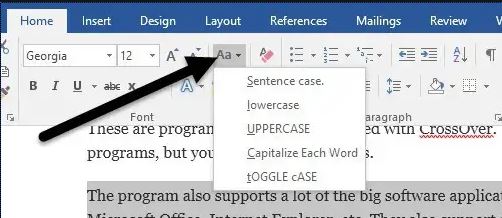
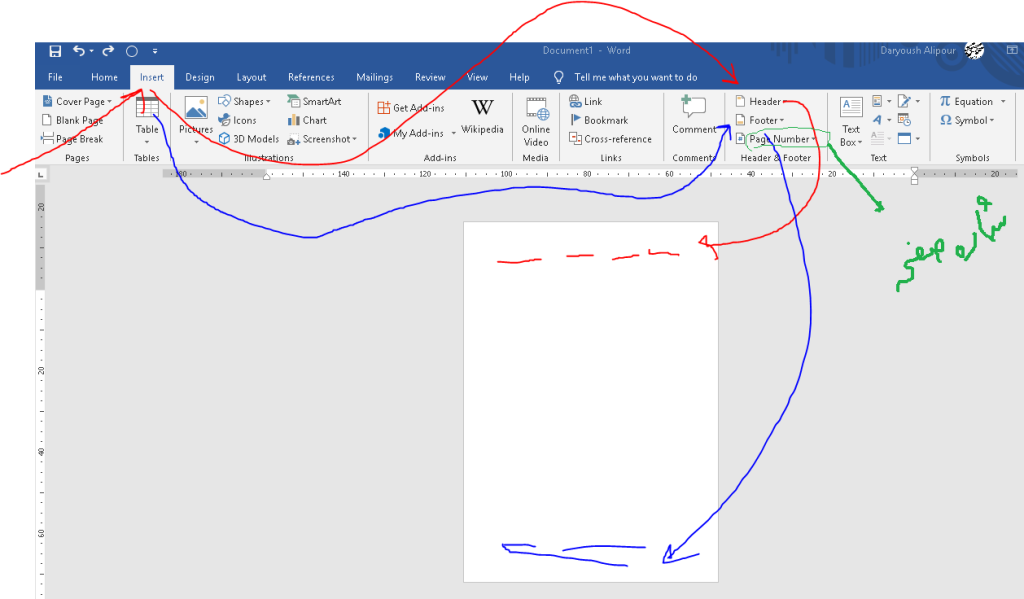
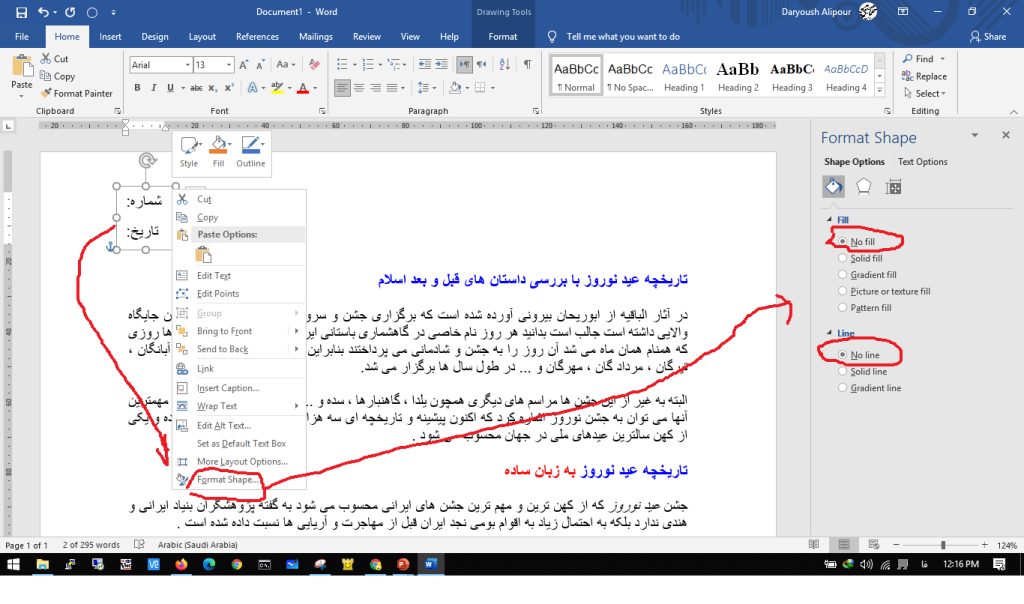
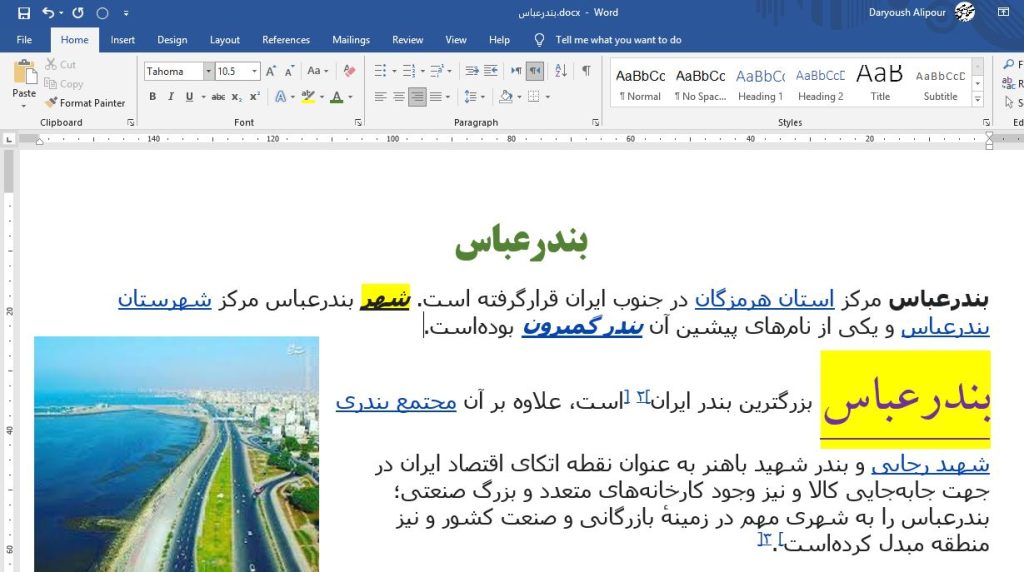
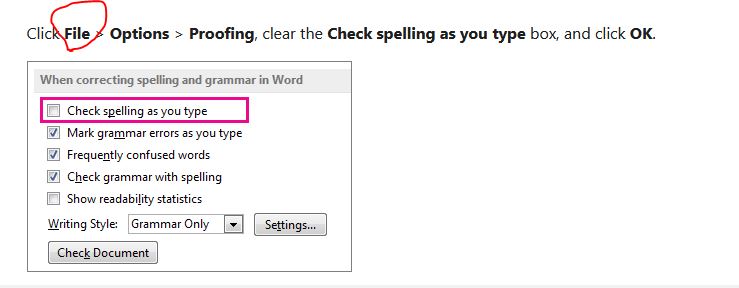
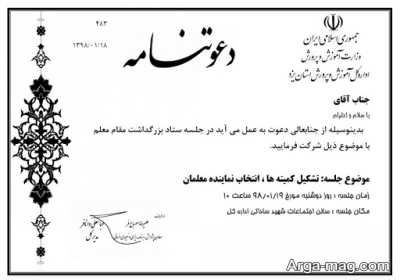
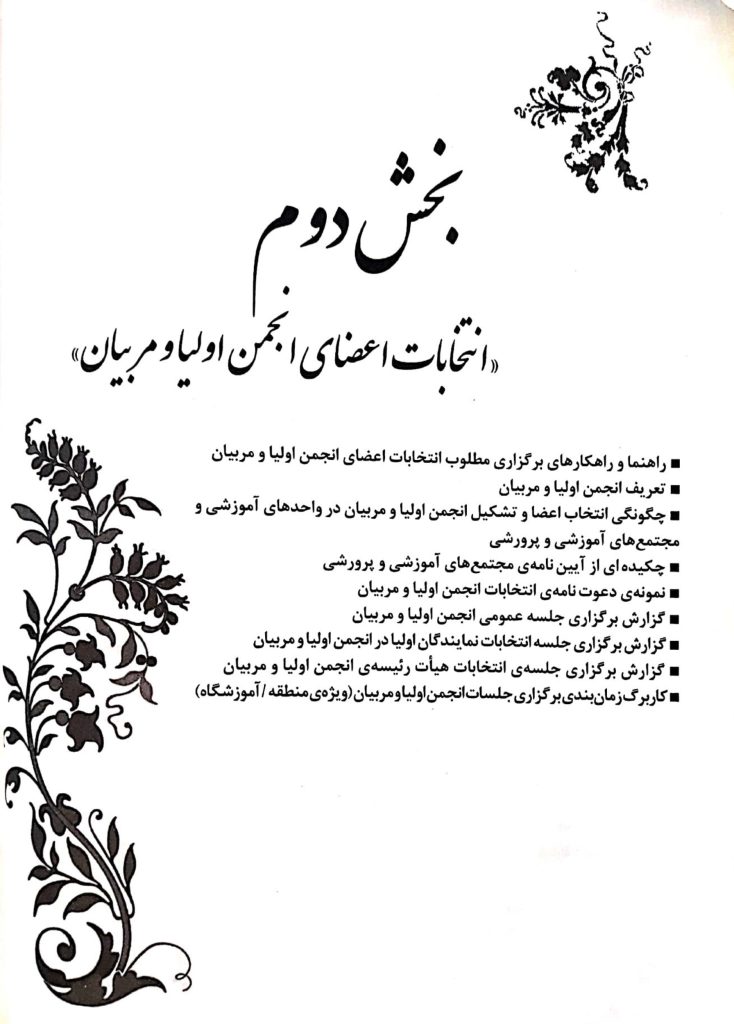
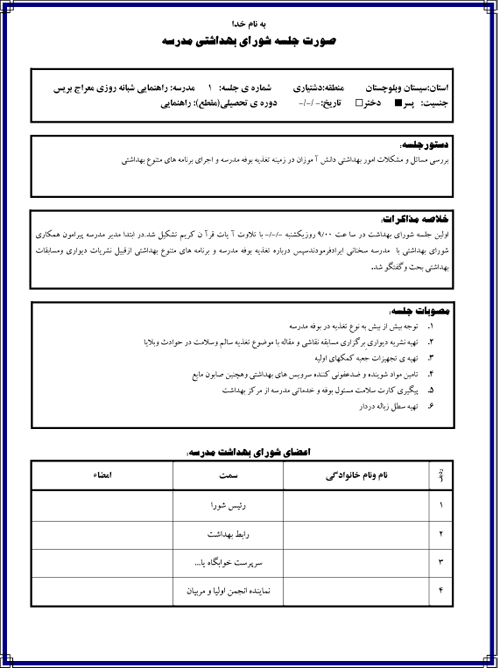
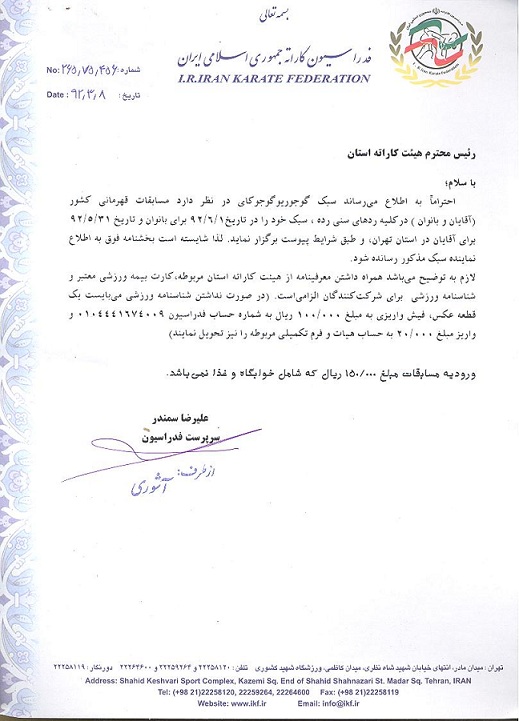

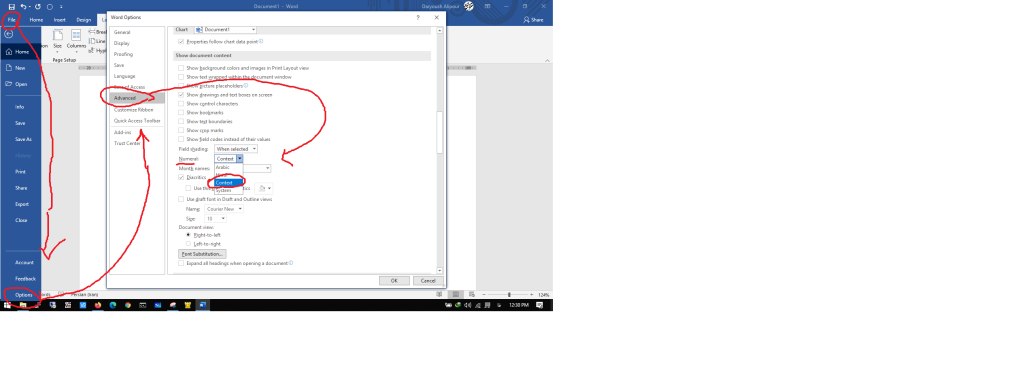
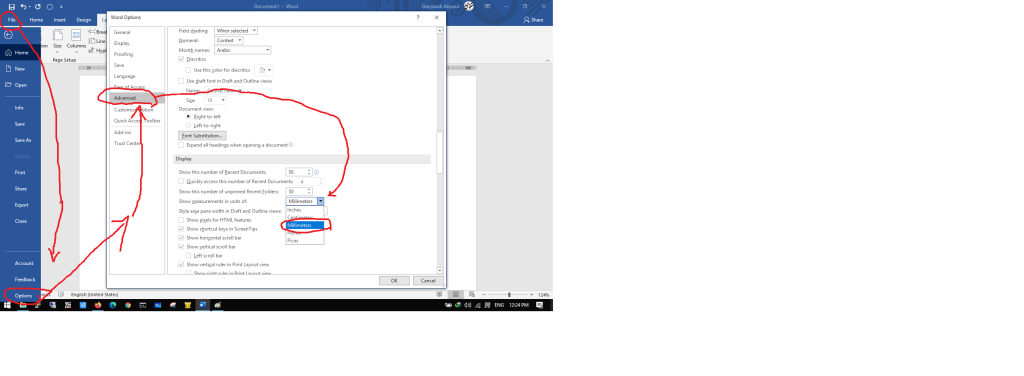
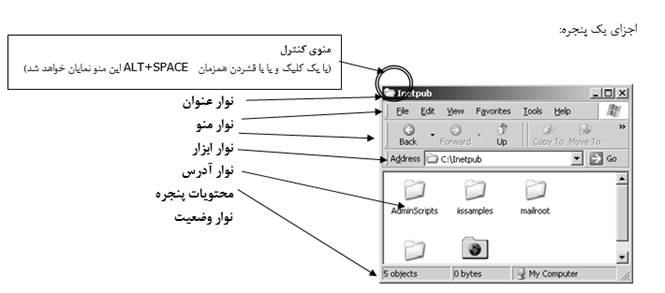
۲- آموزش سيستم عامل ويندوز ICDL۲- آموزش سيستم عامل ويندوز ICDL
آموزشگاه هوش مصنوعی
آموزش سيستم عامل ويندوز – مهارت دوم از ICDL
( استفاده از کامپيوتر و مديريت فايلها )
آشنايي با سيستم كامپيوتر
قاعده نامگذاری درايوها:
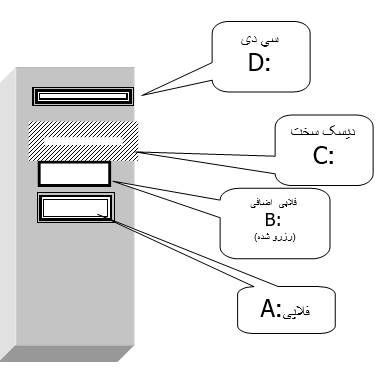
تمرين) کامپيوتر يک اداره دارای ديسک گردانهای فلاپی، ديسک سخت و ديسک نوری میباشد، نام اختصاری ديسک گردانها(درايوها) را نام ببريد.
| FLOPPY DRIVE | A: |
| فلاپی اضافی(رزرو شده) | B: |
| HARD DISK DRIVE | C: |
| CD-ROM DRIVE | D: |
نکته)توسط دستورات خاص نرم افزاری می توان ديسک سخت را طوری قسمت بندی(پارتيشن بندی) نمود که هر قسمت آن همانند يک قسمت مستقل عمل نمايد.
در چنين حالتی بايد توجه داشت که آن قسمتها، با رعايت ترتيب الفبای انگليسی، نامگذاری شده و حرفی پس از آخرين قسمت ديسک سخت، نام سی دی (CD)خواهد بود.
تمرين) کامپيوتر يک مدرسه دارای ديسک گردانهای فلاپی، ديسک سخت 3 قسمتی و ديسک نوری می باشد، نام اختصاری ديسک گردانها(درايوها) را نام ببريد.
| FLOPPY DRIVE | A: |
| فلاپی اضافی(رزرو شده) | B: |
| HARD DISK DRIVE | C: |
| D: | |
| E: | |
| CD-ROM DRIVE | F: |
تمرين) کامپيوتر يک مدرسه دارای ديسک گردانهای فلاپی، ديسک سخت 5 قسمتی و ديسک نوری و دستگاهCD-WRITER می باشد، نام اختصاری ديسک گردانها(درايوها) را نام ببريد.
| FLOPPY DRIVE | A: |
| فلاپی اضافی(رزرو شده) | B: |
| HARD DISK DRIVE | C: |
| D: | |
| E: | |
| F: | |
| G: | |
| CD-ROM DRIVE | H: |
| CD-WRITER | I: |
مفهوم و کاربرد فايل و پوشه
دفتردار يک مدرسه را در نظر بگيريد، او برای هر محصل يک پوشه قرار داده و نام آن محصل را روی آن می نويسد، سپس برخی اسناد متنی(مثلاً کپی شناسنامه) و اسناد تصويری(مثلاً عکس) و … را از آن محصل درخواست نموده و در آن پوشه قرار می دهد و اين پوشه را در کشو و قفسه خاصی قرار داده و ذخيره می سازد. او هر وقت که لازم باشد از اسناد کپی گرفته ويا آنها را جابجا نموده و يا تغييرنام داده و يا حذف می کند. اگر مدير يا کس ديگر اطلاعاتی را راجع به يک محصل لازم داشته باشد، آنگاه دفتردار سريعاً در محل(کشو يا قفسه) مربوطه با توجه به نام آن محصل، پوشه و اسناد موجود در آن را ارايه می دهد.
سيستم بايگانی و بازيابی اطلاعات در کامپيوتر نيز همانند مثال فوق می باشد.
ديسک سخت مرکز بايگانی اصلی سيستم بوده و توسط دستورات نرم افزاری خاصی، می تواند به چند قسمت(پارتيشن) مجزا تقسيم شود. هر سند و مدرک را در کامپيوتر، فايل (file) گويند.
انواع مختلفی از فايلها وجود دارد: (فايل تصويری، متنی، صوتی، برنامه ای) فايلها می توانند در پوشه(شاخه، فهرست،directory ، folder) ذخيره شوند. می توان فايلها را ايجاد کرد، کپی ساخت، تغييرنام داد، جابجا و حذف نمود.
| مقايسه سيستم بايگانی امور دفتری مدرسه با کامپيوتر | |
| دفتر مدرسه | کامپيوتر |
| کشو(قفسه) | درايو(ديسک گردان) |
| پوشه | پوشه، دايرکتوری |
| سند، مدرک | فايل |
هر فايل:
ü دارای نام است.
ü در موقعيت، محل و مسير مشخصی ذخيره شده است.(در ديسکت، ديسک سخت،CD، حافظه RAM ،ROM و نوارهای مغناطيسی)
ü دارای حجم و اندازه ای است.
ü اطلاعات خاصی را نشان می دهد.
با فايلها چه کاری را می توان انجام داد؟
- اجرای آنها ( اگر برنامه باشد)
- مشاهده محتويات آن ( اگر آنها از نوع متنی و تصويری باشند)
- شنيدن آن (اگر صوتی باشد)
- کپی نمودن آن
- انتقال آن
- حذف آن
- ساخت آن
قوانين نامگذاری فايلها :
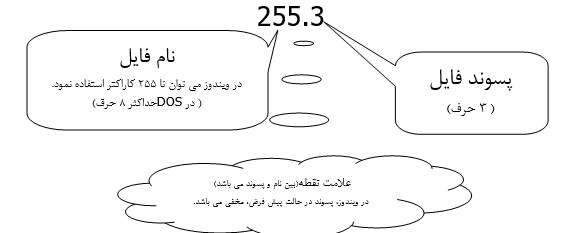
در ویندوز 10، طول حداکثر نام فایل (شامل پسوند) بهطور پیشفرض ۲۵۵ کاراکتر است و طول کامل مسیر (شامل پوشهها + نام فایل) حداکثر ۲۶۰ کاراکتر میباشد. اما از نسخه 1607 به بعد، با فعالسازی گزینه “Enable Win32 long paths” در Group Policy، میتوان این محدودیت را برداشت و طول مسیر را تا ۳۲٬۷۶۷ کاراکتر افزایش داد، به شرطی که فایلسیستم NTFS باشد و برنامهها نیز از مسیرهای طولانی پشتیبانی کنند.
مثال) readme.txt
برخی قوانين نامگذاری فايلها و پوشه ها :
- می تواند ترکيبی از حروف، ارقام و علايم باشد.
- در ويندوز، فاصله مجاز است.
- برخی علايم مجاز نيستند.
راه اندازی:
روالی که با فشردن دکمه روشن نمودن کامپيوتر آغاز شده و تا ظاهر شدن محيط اصلی سيستم عامل ادامه می يابد را راه اندازی (BOOT شدن، بالا آمدن) کامپيوتر گويند.
راه اندازی مجدد کامپيوتر(تمرينی نيست):
گاهی بنا به دلايلی لازم است که در کسری از ثانيه برق کامپيوتر قطع شده و سيستم از نو راه اندازی شود. دو روش برای اين کار وجود دارد:
الف) روش نرم افزاری:
کليدهای CTRL و ALT و DEL همزمان فشرده می شود.
(البته اين روش در محيط ويندوز، برای غيرفعال نمودن يک برنامه در حال اجرا می باشد)
ب) روش سخت افزاری:
فشردن دکمه RESET در جلوی CASE
ورود به محيط كار ويندوز :
با فشردن دکمه روشن در قسمت جلويي CASE عمليات راه اندازی شروع شده و پس از لحظاتی محيط گرافيکی ويندوز ظاهر شده و احتمالاً کادری نمايان می شود و کلمه عبور درخواست می نمايد.
پس از پاسخ دادن به اين کادر، محيط اصلی ويندوز مشاهده خواهد شد.
محيط اصلی ويندوز
| ICON (آيکن ها) |
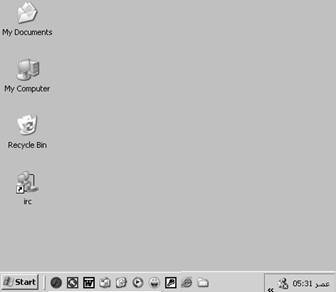
سوال) آيکن های اصلی روی دسک تاپ کدامند؟
| از اين طريق می توان به ديسک گردانهای (درايوهای) مختلف سيستم دسترسي يافت. مثلاً سی دی يا ديسکت | |
| هر گاه برنامه ای را اجرا نموده و در آن برنامه سندی را ايجاد نماييم، آن سند در حالت پيش فرض در پوشه My Documents ذخيره می گردد. ( البته می توان محل ذخيره شدن اسناد را تغيير داد) | |
| هر گاه فايل و يا پوشه ای را حذف نماييم، آن موضوع بطور موقت در پوشه Recycle Bin قرار می گيرد تا ما اين فرصت را داشته باشيم که آن را بازيابی نماييم. |
ايجاد فايل متنی (يادداشت) :
- راست کليک در جای خالی از دسک تاپ
- از منوی باز شده گزينه Newو سپس Text Document را انتخاب می کنيم
- تعيين نامی دلخواه به اين سند جديد
- دابل کليک سند ايجاد شده و تايپ مطالب دلخواه در آن
تمرين) چندين فايل متنی مختلف بسازيد.
ايجاد يك پوشه در محيط DeskTop
1. راست کليک در جای خالی از دسک تاپ
2. انتخاب گزينهNew از منوی باز شده و سپس Folder
3. تايپ نام دلخواه
تمرين) پوشه ای به نام IRAN بسازيد، و سپس يک سند متنی با نام TEL در آن ايجاد نماييد.
نکته) آيکن پوشه ها معمولاً شبيه پوشه های معمولی زرد رنگ می باشد در حاليکه آيکن فايلها به شکل ديگريست ( هر نوع فايل شکل آيکن مشخصی دارد ، به عنوان مثال فايلهای متنی ساده به صورت زير می باشند)

سوال) من يک سند متنی روی دسک تاپ ساخته ام، چگونه می توانم از اين فايل يک کپی در درايو D: قرار دهم؟
پاسخ _ کپی برداری از يک سند :
- راست کليک روی آن سند
- انتخاب گزينه copy از منوی باز شده
- (مشخص نمودن محلی که می خواهيم نسخه کپی در آنجا قرار گيرد.)
- باز نمودن My Computer و سپس درايو D:
- راست کليک در محلی خالی از داخل پنجره بازشده
- انتخاب گزينه paste از منوی باز شده
جابجايي و انتقال يک سند :
- راست کليک روی آن سند
- انتخاب گزينه Move از منوی باز شده
- (مشخص نمودن محلی که می خواهيم سند به آنجا جابجا شود.)
- راست کليک در محلی خالی از داخل پوشه بازشده يا دسک تاپ
- انتخاب گزينه paste از منوی باز شده
تغيير نام يک سند :
- راست کليک روی آن سند
- انتخاب گزينه Rename از منوی باز شده
- تايپ نام دلخواه و سپس فشردن کليد Enter
حذف يک سند :
- راست کليک روی آن سند
- انتخاب گزينه Delete از منوی باز شده
- يک کادر سوالی ظاهر می شود که در صورت اطمينان از حذف Yes را انتخاب می کنيم.
مديريت پنجره ها:
هرگاه روی يک پوشه يا برنامه کليک (دابل کليک) نماييم، آن برنامه در يک پنجره باز خواهد شد.
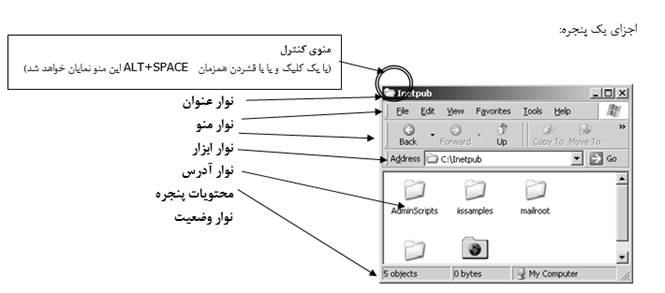
(براي مطالعه) ايجاد يك ميانبر :
می توان بدون کپی نمودن يک پوشه يا فايل، آيکن ميانبر آن را در محل دلخواه قرار داد.
يک روش ساده نگه داشتن دکمه راست روی موضوع دلخواه و سپس Drag کردن است.
راه ديگر:
- Copy موضوع موردنظر
- انتخاب Paste Shortcut ازمنوی راست کليک در محلی خالی
(براي مطالعه) فرمان Send To ( فرستادن به…. )
برای کپی نمودن سريع يک پوشه يا فايل، ابتدا روی آن کليک نموده و سپس از گزينه Send To يکی از موارد زير را انتخاب می نماييم.
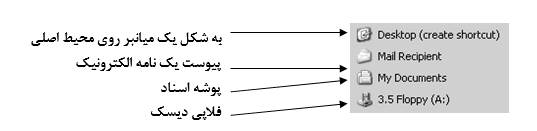
(براي مطالعه) نكاتي راجع به محيط سطل بازيافت:
- هرگاه فايل يا پوشه اي را حذف نماييم، تحت شرايطي در سطل قرار مي گيرد و ما اين فرصت را خواهيم داشت تا آن را برگردانيم (گاهي بازيابي ممكن نخواهد بود)
- براي بازيابي موضوع حذف شده، ابتدا سطل را باز نموده و سپس روي مورد دلخواه راست كليك نموده و گزينه Restore را انتخاب مي نماييم.
- براي تغيير تنظيمات سطل بازيافت، روي آن راست كليك نموده و گزينه Properties را انتخاب مي نماييم تا كادر مربوطه ظاهر گردد. سربرگ اول اين كادر براي تنظيمات كلي و عمومي مي باشد.
- گزينه هاي زير در برگه نخست كادر خصوصيات قابل تنظيم است:
| Configure drives independently | پيكربندي درايوها بطور مستقل و جداگانه |
| Use one setting for all drives | استفاده از يك تنظيمات براي همه درايوها |
| Do not move files to the Recycle Bin | فايلها هنگام حذف نابود شده و وارد سطل نگردند |
| با حركت دادن اين زبانه قادريم ظرفيت سطل را تغيير دهيم | |
| Display delete confirmation dialog | نمايش كادر پرسشي هنگام حذف |
(براي مطالعه) تنظيم خصوصيات صفحه نمايش در ويندوز :
در جايي خالي از Desktop راست كليك نموده و گزينه Properties را انتخاب مي نماييم تا كادر مربوطه ظاهر شود. اين برگه ها عبارتند از:
| برگه Back Ground | تغيير تصوير پس زمينه |
| برگه Screen Saver | تنظيم يك قطعه نمايشي به عنوان محافظ صفحه نمايش براي زمان بيكار ماندن سيستم |
| برگه Appearance | تغيير جزء خاصي از ويندوز و يا تنظيم يك الگو براي دگرگون ساختن كل محيط ويندوز |
| برگه Effects | تغيير شكل آيكنهاي اصلي و … |
| برگه Web | فعال و اينترنتي نمودن ظاهر دسك تاپ (با تك كليك برنامه ها اجرا مي شوند |
| برگه Setting | تنظيمات رنگ و كيفيت وضوح صفحه نمايش و… |
چگونگي جستجوي فايل ها يا پوشه ها:
از طريق منوي Start و يا با راست كليك روي پوشه دلخواه مي توان برنامه Find را اجرا نمود.

قسمتهاي مهم برگه اول كادر Find
| تايپ نام و مشخصه فايل يا پوشه مورد نظر ( بعنوان مثال *.jpg براي يافتن تمامي تصاوير با هر نامي و با پسوند jpg ) | Named |
| اگر فايل متني خاصي را بخواهيم جستجو نماييم كه حاوي كلمه خاصي باشد آن كلمه را اينجا تايپ مي نماييم ( اغلب لازم نيست) | Containing text |
| تعيين محل جستجو ( مثلاً درايو C: ) | Look in |
برنامه كمكي و راهنما:
با انتخاب Help از منوي Start مي توان در كتابچه راهنماي ويندوز، درباره برنامه ويندوز، اطلاعات مختصر و مفيدي را به زبان روان و ساده انگليسي پيدا نمود.
كادر اين برنامه داراي سه برگه مي باشد:
| در سمت چپ، ليست درختي بخشهاي مختلف كتابچه مشاهده مي شود كه با كليك روي نماد كتابچه هر بخش، يك ساختار درختي فرعي ظاهر مي شود، و ما موضوع موردنظر را انتخاب نماييم (دابل كليك روي آيكن علامت سوال) تا در سمت راست اطلاعات مربوطه ظاهر شود. | Contents |
| جستجوي الفبايي (حرف يا حروف اول كلمه را در قسمت مشخص شده بالاي برگه تايپ مي نماييم و سپس روي كلمه يافته شده در پايين دابل كليك مي كنيم و اطلاعات مربوط به آنرا در سمت راست مطالعه مي نماييم) | Index |
| تايپ عبارت مورد نظر (مثلاً paint براي كسب اطلاعات درباره برنامه نقاشي) | Search |
برنامه ويرايشگر ويندوز:
Start 8 Programs 8 Accessories 8 Wordpad
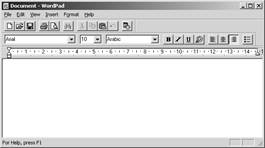
Tool bar (نوار ابزار)
| New | ايجاد سند جديد | |
| Open | باز نمودن سند موجود (قبلاً ذخيره شده) | |
| Save | ذخيره سند | |
| چاپ سند | ||
| Print prieview | پيش نمايش چاپ | |
| Find | جستجو و يافتن يك عبارت در سند فعلي | |
| Cut | برش متن انتخاب شده جهت انتقال آن به جايي ديگر از سند | |
| Copy | كپي متن انتخاب شده | |
| Paste | چسباندن مطالب copy و يا cut شده | |
| Undo | لغو آخرين فرمان | |
| Date/Time | درج ساعت و تاريخ فعلي سيستم در محل مكان نما |
Format bar (نوار قالب بندي)

| Font | نوع قلم | |
| Font size | اندازه قلم | |
| Font Script | نوع اسكريپت قلم | |
| Bold | ضخيم و پررنگ شدن قلم | |
| Italic | كج و مايل شدن قلم | |
| Underline | زير خط دار شدن قلم | |
| Color | رنگ قلم | |
| Align left | (چپ چين) تراز شدن متن از چپ | |
| Center | وسط چين | |
| Align right | راست چين | |
| Bullets | علامتگذاري ليستها |
(مرور درس) پرسش و پاسخ :
ICON چيست؟
يك نماد با زيرنويس كه نمايانگر يك فايل و يا پوشه مي باشد.
شخصي قصد دارد در كامپيوتر خود تعداد زيادي عكس، متن، موسيقي و فيلم قرار دهد، از نظر فني چه توصيه اي براي ايشان در نظر داريد؟
- ديسك سخت چند قسمتي باشد. و درايو C: را كاري نداشته باشيد ( يا هر درايوي كه سيستم عامل آنجاست)
- اگر تعداد درايوها زياد باشد، بد نيست هر درايو را براي ذخيره يك موضوع تعيين نماييد.
- براي هر موضوع پوشه اي ساخته و در صورت نياز درون هر پوشه، زيرپوشه هايي ايجاد نماييد.
- نامگذاري پوشه ها طوري باشد كه بعدها فقط با ديدن نام آنها متوجه محتويات آن شويد.
- …
كپي، انتقال و حذف فايلها چگونه انجام مي گيرد؟
COPY 8 PASTE كپي
CUT 8 PASTE جابجايي
DELETE حذف
قصد داريم تمامي موسيقي هاي با قالب بندي mp3 را در يك كامپيوتر بيابيم. راه حل چيست؟
در برگه اول برنامه FIND وقسمت بالا *.MP3 را نوشته و در پايين ترين ليست بازشونده MY COMPUTER را انتخاب نموده و كليد ENTER را فشار دهيد تا ليست اين فايلها نمايان شود
(توجه داشته باشيد كه ممكن است سيستم طوري تنظيم شده باشد كه فايلهاي با خصلت مخفي نمايش داده نشوند)
درباره برنامه PAINT مطالبي توضيحي و كمكي را به زبان انگليسي نشان دهيد.
برنامه HELP
يك سند متني با مندرجات دلخواه ايجاد نموده و پس از آن در درايو D: با نام APA ذخيره نماييد.
از منوي FILE در برنامهWORDPAD و در كادر SAVE AS از ليست بازشونده بالايي محل ذخيره شدن را مشخص ساخته و در قسمت مربوط به NAME نام دلخواه را به فايل اختصاص مي دهيم.
چاپ اسناد مختلف به چه نحو است؟
از منوی FILE برنامه موردنظر گزينه PRINT را انتخاب و تاييد میکنیم.
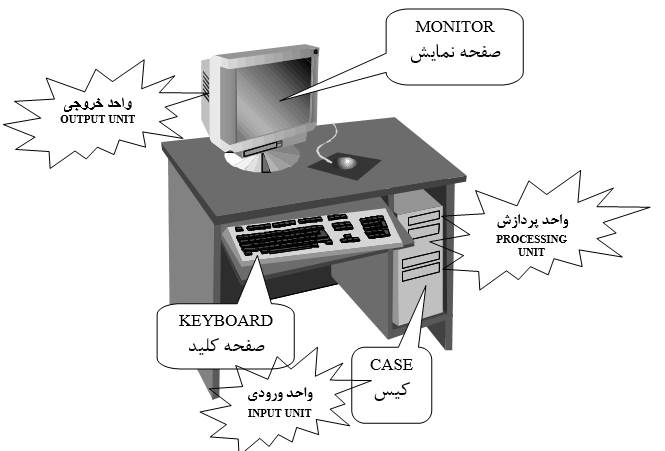
۱- مفاهيم اوليه و اساسی کامپيوتر ICDL۱- مفاهيم اوليه و اساسی کامپيوتر ICDL
1
آموزشگاه هوش مصنوعی
tirotir.ir
مفاهيم اوليه و اساسی کامپيوتر
تعريف و مزايای کامپيوتر:

شما با تلويزيون خود آشنايي داريد، و ممکن است که به آن تا حدودی وابسته باشيد! تلويزيون رايج ترين دستگاه خروجی محسوب می شود. اين بدين معنی است که از تلويزيون مطالبی پخش شده و شما احتمالاً از آن استفاده نموده ايد.
از طريق دستگاه کنترل می توان به تلويزيون ورودی داد،به عنوان مثال کانالها را تغيير داده، صدا، رنگ و برخی موارد ديگر را عوض نمود. در واقع منظور از اصطلاح خروجی يعنی گردش اطلاعات به سمت شما و ورودی يعنی گردش اطلاعات از سوی شما به يک دستگاه خاص.
کامپيوتر يک دستگاه الکترونيکی است که روی موضوعاتی که به آن می دهيم(از طريق واحد ورودی) کار کرده و اطلاعات موردنظر را ارايه می نمايد(توسط واحد پردازش).
قسمتهای مختلف کامپيوتر:
- قسمتهايي که ورودی را دريافت می نمايند.
- قسمتهايي که روی موضوعات ورودی عملياتی خاص انجام می دهند.
- قسمتهايي که خروجی را ارايه می نمايند.
- قسمتهايي که مطالب و موضوعات را حتی هنگام خاموشی کامپيوتر، ذخيره و نگهداری می نمايند.
برخی مزايای کامپيوتر عبارتند از :
- سرعت، اطمينان، دقت ، حافظه بالا و …
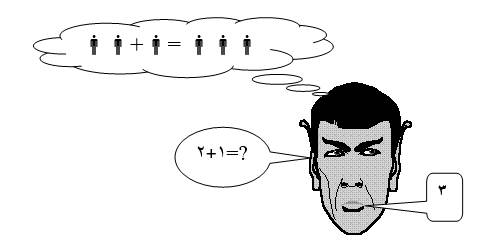
در شکل فوق واحدهای ورودی، پردازش و خروجی را نام ببريد.
آشنايي با انواع کامپيوترهای شخصی:
1. کامپيوتر روميزی
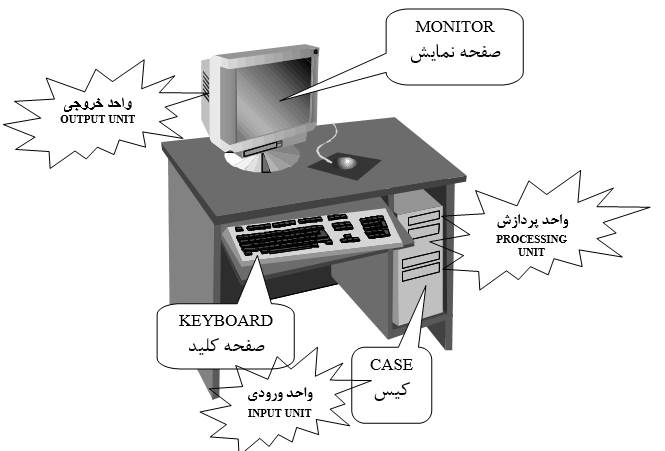
2. کامپيوتر قابل حمل (لپتاپ)
کامپيوتر هايي می باشند که بطور كامل درونی مخصوص قرار گرفته و قابل حمل و جابجايي هستند.
اين کامپيوترها نسبت به نوع معمولی، بسيار گران می باشند.

آشنايي با علوم کامپيوتر:
سخت افزار(HARDWARE)
آنچه از کامپيوتر که از نظر فيزيکی قابل لمس می باشد، سخت افزار است. مثل مانيتور، چاپگر، ماوس و …
نرم افزار(SOFTWARE)
برنامه های کامپيوتر مثل بازيها، برنامه نقاشی، برنامه نقشه کشی و … را نرم افزار گويند.

ميان افزار(FIRMWARE)
حدواسط بين سخت افزار و نرم افزار
(برنامه ها و دستورالعمل هايي خاص، در سخت افزاری ويژه می باشد مثل Rom Bios)
آشنايي با اصطلاحات ويژه سيستم کامپيوتری:
تعريف سيستم و سيستم کامپيوتری :
مجموعه ای از اعضاء يک مجموعه که بطور هماهنگ کار کنند و هدف مشخصی داشته باشند، يک سيستم محسوب می شوند.
تعريف داده (DATA) :
مواردی که به کامپيوتر داده می شوند تاروی آن عمليات انجام دهد را داده گويند.
تعريف پردازش(PROCESSING) :
عملياتی که کامپيوتر روی داده ها انجام مي دهد.
تعريف اطلاعات(INFORMATION) :
حاصل پردازش روی داده ها می باشد.
نمای جلوی CASE :
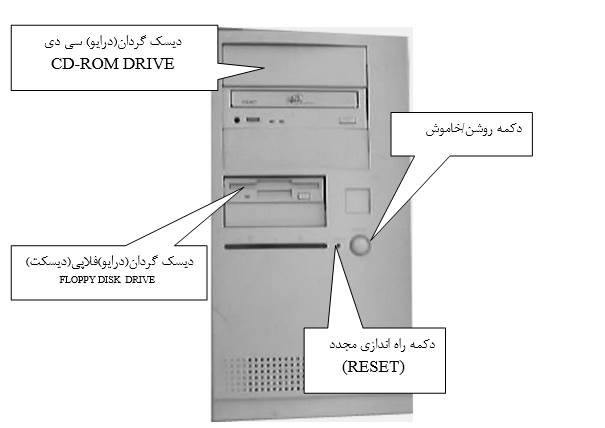
نمای پشت CASE :
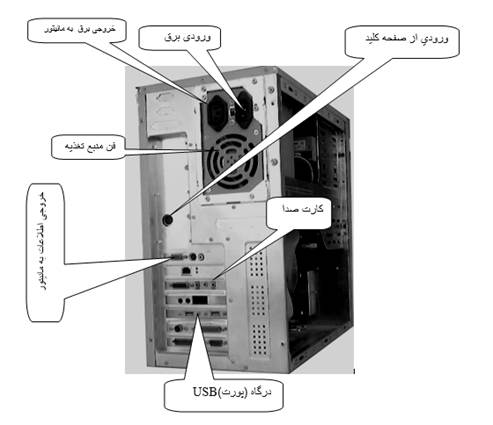
درگاهها(PORTS)
محلهايي در پشت CASE بوده که دستگاههای مختلف مثل چاپگر، اسکنر، ماوس و غيره از طريق آن به بورد اصلی کامپيوتر و صل می شوند.
انواع مختلفی از درگاهها وجود دارد:
- سريال يا سری(COM1,…) بصورت 25 و 9 سوزنه وجود دارد(ارسال داده ها بيت به بيت)
- موازی يا پارالل(LPT1,…) بصورت 25 سوراخه بوده و اغلب برای چاپگر استفاده می شود.
- USB برای اکثر دوربين های اينترنتی، چاپگر و …
- INFRARER(بی سيم)
نمای داخلCASE :

آشنايي با انواع کامپيوتر بر اساس قدرت پردازش و کاربرد آن
INTEL Paragom XP/S Super Computer
$1.2 million dollors in 1994
(سال 1994 قيمت اين ابرکامپيوتر بيش از يك ميليون دلار بوده است)

INTEL iPSC Super Computer
$750.000 dollors in 1985
(قيمت اين ابرکامپيوتر حدود هفتصد هزار دلار بوده است)
- کامپيوترهای شخصیPersonal computer (pc)
- کامپيوترهای کوچک Mini computer
- کامپيوترهای بزرگ Main frame
- ابر کامپيوترها Super computer
آشنايي با ساختار عمومی يک کامپيوتر شخصی
Case
واحد پردازش سيستم بوده و اصلی ترين قسمت می باشد.
دو نوع Case وجود دارد:
الف) افقی يا تخت(رو ميزی)
ب) عمودی يا قائم
POWER SUPPLY
منبع تغذيه سيستم است.
(برق شهر را گرفته و به قطعاتی که بدان نيازمندند بحد لازم توزيع می کند)
Cpu (واحد پردازش مرکزی) و اجزای داخلی آن
ريز پردازندهMicroprocessor)) يا cpu (central processing unit) نوعی مدار مجتمع يا ic می باشد که روی برد اصلی(مادر برد) قرار گرفته و سيستم را مديريت نموده و عمليات رياضی، محاسباتی و منطقی را انجام می دهد.
- cu واحد کنترل(control unit)
- Alu واحد محاسبات و منطق (arithmetic & logic unit)
- register ثبات(نوعی حافظه است)
(درون CPU حافظه ديگری به نام CACHE وجود دارد که واسطه ای است بين RAM و آن)
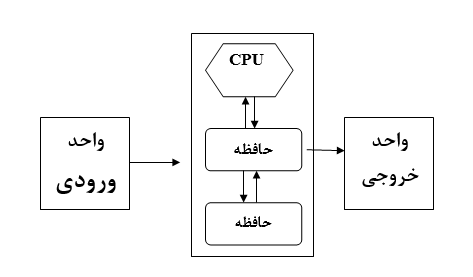
بخشهای مرتبط با cpu
حافظه اصلی _ حافظه جانبی _ واحد ورودی _ واحد خروجی
دياگرام عمومی يک کامپيوتر شخصی
2
شناخت حافظه و کاربرد آن
زمانيکه برنامه ها از DISK به RAM منتقل شوند، آنگاه آماده اجرا خواهند شد.
اگر در يک برنامه واژه پرداز، حرفی را تايپ نماييد، آن حرف در حافظه RAM قرار خواهد گرفت و اگر کامپيوتر خاموش شود، آن حرف پاک می شود. ولی اگر در ابتدا آن حرف را در يکی از انواع حافظه جانبی، ذخيره (save) نماييد، آنگاه با خاموشی کامپيوتر، آن حرف پاک نخواهد شد.
- وقتی گفته می شود که کامپيوتر با 0 و 1 کار می کند. منظور اين نيست که درون آن خود اعداد 0 و 1 وجود دارند بلکه منظور استفاده از يک سيستم دو حالته است.
به مثال زير توجه نماييد:
| براي مطالعه: شما و دوستتان با الفبای دو حالته 0 و 1 يک جدول رمز مشابه زير بسازيد و سپس سعی نماييد پيامهايي را ردوبدل نماييد. |
| 00111 الف 01000 ت 01100 س 11100 ن 10101 ش 10001 ل 10111 د 10010 ر … … |
| تمرين) منظور از عبارات زير چيست؟ |
| 01100 10010 10111 ð سرد |
| 01000 00111 10010 ð تار |
| 10111 11100 10111 00111 11100 ð دندان |
| پس قبول داريم که با الفبای دو حرفی نيز می توان به تبادل نظر و رد و بدل پيام دلخواه پرداخت. حالا دقت نماييد که هر موضوع دو حالته را می توان به 0 و 1 تعبير نمود. |
| صدای زير 0 صدای بم 1 ملاحظه بفرماييد: قرارداد در تلگراف و الفبای مورس (البته بجای 0و1 از نقطه(.) و خط(_ ) استفاده می شود) |
| نور پايين 0 نور بالا 1 در ديسکت و ديسک سخت از مغناطيس استفاده شده است. |
| – 0 + 1 در حافظه RAM از الکترونيک و الکتريسيته استفاده شده است. |
| دشارژ 0 شارژ 1 |
| در CD از حفره و عدم حفره استفاده شده است. |
| عدم حفره 0 حفره 1 |
آشنايي با واحدهای حافظه
کوچکترين جزء و عنصر حافظه را bit (ذره، لقمه، رقم دودويي) گويند. هر bit دو حالت دارد:
يک و صفر (به عبارتی ديگر يک بيت، يا 1بوده ويا 0 است.
بيتها بصورت هشت تايي گروه بندی می شوند که به هر گروه هشت تايي، يک بايت (BYTE) گويند. هر بايت يک کاراکتر(حرف، رقم، علامت) را نشان می دهد.
صفر و يکها ممکن است در 256 حالت متفاوت، و در يک گروه هشت تايي آرايش يابند.(معادل 28 )
(چند حالت ممکن را با توجه به شکلهای زير توجه نماييد)
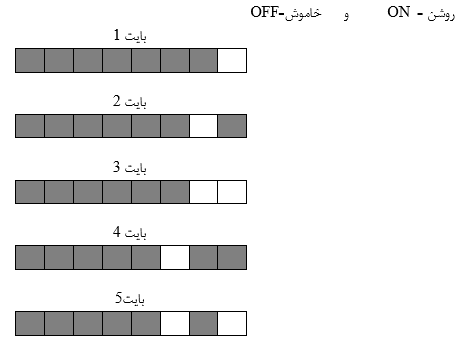
| Bit | کوچکترين جزء حافظه |
| Byte (اختصاراً بايت) | ترکيبی از هشت بيت |
| Word | معمولاً دو بايت |
| Kb کيلوبايت | 1024 B |
| Mb مگا بايت | 1024 KB |
| Gb گيگا بايت | 1024 MB |
| Tb ترا بايت | 1024 GB |
| Pb پتا بايت | 1024 TB |
| Eb اگزا بايت | 1024 PB |
| نوع حافظه جانبی | ظرفيت |
| ديسکت(FLOPPY)سه و نيم اينچی | 1.44 MB |
| ديسک نوری(CD-ROM) | 650 – 700 MB |
| ديسک سخت(HARD DISK) | دهها گيگا بايت |
انواع حافظه
الف) اصلی ب) جانبی (کمکی يا ثانوی) اصول شناخت حافظه اوليه يا اصلی و کاربرد آن
Ram
اطلاعات را تا زمانيکه کامپيوتر روشن است در خود ذخيره می نمايد و هنگامی که لازم باشد آن را در دسترس قرار می دهد، هم می توان در آن نوشت و هم از آن خواند.
Rom
نوعی حافظه فقط خواندنی بوده و اطلاعات درون آن دايمی و پايدار می باشد.
(با خاموشی کامپيوتر اطلاعات درون آن پاک نمی شوند)
انواع مختلفی از اين نوع حافظه وجود دارد:
PROM (قابل برنامه نويسی)
EPROM (قابل پاک شدن توسط اشعه ماوراء بنفش)
EEPROM (قابل پاک شدن توسط جريان الکتريسيته)
توانايي شناخت حافظه ثانويه يا جانبی و کاربرد آن
Floppy disk
به شيوه مغناطيسی داده ها را ذخيره می نمايد (+ يک / – صفر)
درون قاب آن، صفحه پلاستيکی آغشته به اکسيد آهن که مغناطيس شونده است، قرار دارد.
امروزه نوع 5/3 اينچی با ظرفيت 44/1 مگابايت آن متداول است.
Hard disk
چند صفحه از جنس آلياژ آلومينيوم، بطور هم محور، با هدهای خواندن و نوشتن، در محفظه ای مخصوص قرار گرفته و ديسک سخت را تشکيل می دهند.(انبار اصلی کامپيوتر با ظرفيت دهها گيگا بايت است)
Cd rom
توسط اشعه ليزر عمليات خواندن و نوشتن در آن صورت می پذيرد.
به آن ديسک نوری يا ليزری نيز گويند. بين 650 تا 700 مگابايت ظرفيت دارد.
فقط خواندنی بوده و با دستگاه WRITER می توان درون آن نوشت
DVD
مشابهCD بوده ولی ظرفيتی چند برابر دارد.
TAPE
نوار مغناطيسی(مشابه نوارهای معمولی ضبط صوت)
در برخی مراکز برای پشتيبان گيری از اطلاعات استفاده می شود.
دسترسی مستقيم و ترتيبی
بطور کلی به دو شيوه می توان اطلاعات را ذخيره و يا بازيابی نمود.
الف) دسترسی ترتيبی:
همانند کتابهای موجود در يک کتابخانه، که با ترتيب خاصی بايگانی شده ويا بازيابی می شوند.
يا در يک کاست موسيقی که در صورت علاقه به قسمت خاصی از اين کاست، بايد با صرف زمانی نه چندان کوتاه، آن قسمت را بيابيم.
حافظه های جانبی کامپيوترها در گذشته ترتيبی بوده اند : نوارهای مغناطيسی، کارت پانچ و نوارهای کاغذی
ب)دسترسی مستقيم يا تصادفی:
در فلاپی، ديسک سخت و CD-ROM سيستم بايگانی و بازيابی اطلاعات ترتيبی نيست، به عنوان مثال اگر عکس خاصی را بخواهيم ذخيره و يا مشاهده نماييم، با دانستن نام آن، سريعاً عمليات لازم را انجام می دهيم.
انواع دستگاههای ورودی و کاربرد آن
کارت صدا :
برای استفاده از امکانات صوتی، بايد حتماً کامپيوتر کارت صدا داشته باشد. اين کارت همانند ديگر کارتها، درون شکافهايي مخصوص، درون CASE و روی بورد اصلی قرار گرفته و اين امکان را به ما می دهد تا بلندگو (SPEAKER) و ميکروفن را به آن وصل نماييم.
برخی کليدهای ويژه صفحه کليد:
| Enter | دو کاربرد دارد | تاييد نهايي يک فرمان | |
| ايجاد و اضافه نمودن يک سطر خالی در برنامه های واژه پرداز | |||
| Shift | دو کاربرد دارد (درصورتيکه اين کليد را همزمان نگهداريد) | بزرگ تايپ شدن حروف انگليسی | |
| تايپ علامت بالايي کليدهای دوعلامته | |||
| Space | ايجاد فاصله هنگام تايپ (همچنين انتخاب يا لغوانتخاب يک گزينه در برخی برنامه ها) | ||
| ß Back space | پاک نمودن کاراکتر(حرف، رقم، علامت) قبلی | ||
| Ctrl | يک کليد ترکيبی است(در برخی برنامه ها همزمان با کليدی ديگر فشرده شده و عمليات خاصی را سبب می گردد مثلاً Ctrl+C که برای لغو برخی برنامه های در حال اجرا کاربرد دارد) | ||
| Alt | يک کليد ترکيبی است | ||
| برای ايجاد فاصله بيشتر در هنگام تايپ کاربرد دارد(در برخی برنامه ها برای انتقال مکان نما از يک قسمت به قسمت ديگر بکار می رود) | |||
| Esc | پاک نمودن کادر های باز در برخی برنامه ها | ||
| Del | حذف کاراکتر فعلی | ||
| ← | حرکت مکان نما به چپ | ||
| ↑ | حرکت مکان نما به بالا | ||
| → | حرکت مکان نما به راست | ||
| ↓ | حرکت مکان نما به پايين | ||
| Home | حرکت مکان نما به ابتدای سطر جاری | ||
| End | حرکت مکان نما به انتهای سطر جاری | ||
| Ctrl+Home | حرکت مکان نما به ابتدای سند | ||
| Ctrrl+End | حرکت مکان نما به انتهای سند | ||
| PgUp | حرکت مکان نما يک صفحه به بالا | ||
| PgDn | حرکت مکان نما يک صفحه به پايين | ||
| Pause | توقف و مکث اجرای برخی برنامه ها تا هنگامي که کليد دلخواهی از صفحه کليد فشرده شود ( مثلاً هنگام راه اندازی کامپيوتر برای اينکه مشخصات سخت افزاری سيستم را مشاهده نمود می توان اين کليد را فشرد و اطلاعات روی صفحه را مطالعه نمود) | ||
| PrtScr | چاپ صفحه نمايش در محيط برنامه DOS از محيط برنامه WINDOWS عکس می گيرد (در برنامه نقاشی و از منوی EDIT گزينه PASTE را انتخاب نماييد تا عکس گرفته شده ظاهر شود) | ||
| ÿ | کليد ويندوز(WinKey) در محيط ويندوز کاربرد دارد. | ||
MOUSE
دستگاهی ورودی است که در کامپيوترهای امروزی الزامی می باشد.
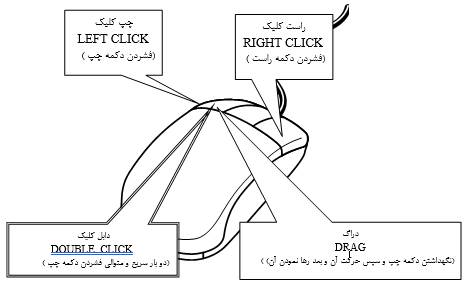
JOYSTICK
(اهرم هدايت، دسته بازی)
دستگاهی ورودی است که برای بازيهای کامپيوتری مورد استفاده قرار می گيرد.
SCANNER (پويشگر) و انواع آن
دستگاهی ورودی بوده که کپی تصاوير را ديجيتالی نموده و به کامپيوتر می فرستد.
(می توان بر حسب واحد DPI کيفيت را تنظيم نمود، در ضمن 300DPI کيفيت مناسبي برای کارهای چاپی است)
| اسکنر تخت | اسکنر دستی |
مودم
می دانيم که دو نفر از فاصله دور می توانند با هم ارتباط همزمان داشته باشند و اين نيز مشخص است که هر نفر به يک دستگاه تلفن احتياج دارد.
کامپيوترها نيز مي توانند از راه دور ارتباط يافته و اطلاعات مختلف را رد و بدل نمايند. البته هر کامپيوتر به دستگاهی به نام MODEM نياز دارد.
مودم اطلاعات ديجيتال کامپيوتر را از طريق خط تلفن به کامپيوتر ديگر ارسال می نمايد و در کامپيوتر ديگر مودمی ديگر قرار دارد که اطلاعات را از خط تلفن گرفته و بصورت ديجيتال در می آورد.
مودم انواع مختلفی دارد:
- داخلی(INTERNAL) – داخل CASE قرار دارد.
- خارجی (EXTERNAL) – خارج از CASE قرار دارد.
- مخصوص کامپيوترهای قابل حمل(PCMCIA)
دوربين ديجيتال
دستگاهی ورودی بوده، انواع مختلفی دارد و در اينترنت و همچنين در امور تبليغاتی کاربرد فراوانی دارد.
اغلب پس از نصب برنامه مربوطه، توسط کابلی، از طريق درگاه USB به پشت CASE وصل می شود و اين قابليت را دارد که بطور همزمان فيلم را نشان داده و تعدادی عکس را در حافظه خود، ذخيره نمايد.
در قسمت بالايي تصوير زير ، دستگاه ورودی جديدی مشاهده می شود که حرکات دست را شبيه سازی می نمايد و در صنعت و پزشکی کاربرد دارد.
و در قسمت پايين همين تصوير، دستگاه سه بعدی سازی تصوير ملاحظه می گردد.
انواع دستگاههای خروجی و کاربرد آن
چاپگرها:
PLOTTER
دستگاهيست برای چاپ نقشه های فنی و پيچيده
MONITOR و انواع آن
(معروفترين خروجی کامپيوتر است)
CRT
پيکسل(PIXEL):
کوچکترين جزء تصوير را پيکسل گويند.
رزولوشن(RESOLOTION):
منظور کيفيت و وضوح تصوير(ريز و درشتی)است.
MOTHER BOARD و اجزای تشکيل دهنده آن
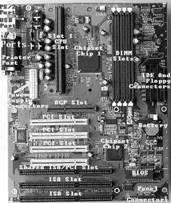
SLOT يا SOCKET ويژه CPU را گاهی سوکت ZIF می نامند.
- SLOT ويژه RAM.
- کارت گرافيک اغلب در شکاف AGP قرار می گيرد.
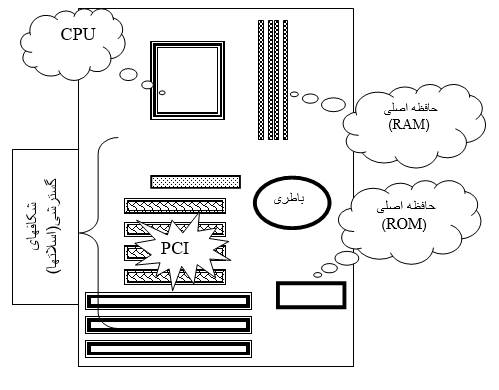
| انواع گذرگاه (BUS) | DATA BUS | ارسال داده ها بين RAM و وسايل ورودی و خروجی |
| CONTROL BUS | ارسال سيگنالهای کنترلی به قسمتهای مختلف | |
| ADDRESS BUS | ارسال آدرس اطلاعات موجود در حافظه RAM |
نرم افزار
انواع نرم افزار:
الف) نرم افزار سيستمی
سيستم عامل ها (مثل Windows98)
برنامه های کمکی و سودمند) مثل (NC
مترجمها، مفسرها و زبانهای برنامه نويسی
ب) نرم افزار کاربردی واژه پردازها (مثل WORD)- صفحه گسترده (مثل EXCEL)- گرافيک (مثل PHOTOSHOP)
انيميشن (مثل 3D STUDIO)- نقشه کشی (مثل AUTOCAD)- بانک اطلاعاتی (مثل ACCESS)- بازيها و غيره
شناخت سيستم عامل و کاربرد آن
همانطوريکه CPU قلب سخت افزار است، سيستم عامل قلب نرم افزار می باشد.
سيستم عامل برنامه ای است واسطه و سلطه گر
سيستم عامل برنامه ای است که با روشن شدن کامپيوتر کليه امور را تحت نظارت و کنترل قرار داده و تا زمان خاموشی سيستم، فرمانها و دستورالعملهای آن، شرايطی را فراهم می سازد تا کاربر عمليات لازم را انجام دهد، و اگر سيستمی فاقد سيستم عامل باشد همانند ماشين بدون بنزين بوده و نمی توان از آن سيستم استفاده نمود.
يک چهارراه بسيار شلوغ را تجسم نماييد که برای جلوگيری از تصادفات و ترافيک، به پليس راهنمايي احتياج باشد. سخت افزار و نرم افزارهای ديگر نيز به سيستم عامل احتياج دارندتا همانند پليس راهنمايي، در مديريت وکنترل امور نقش ايفا نمايد.
اين پليس اگر يک سرباز باشد و يا يک افسر، با توجه به تجربه او کارآيي فرق خواهد داشت. کيفيت سيستم عامل ها نيز متفاوت است، مثلاً DOS سيستم عاملی به مراتب ضعيفتر و محدودتر از سيستم عامل WINDOWS 98 است.
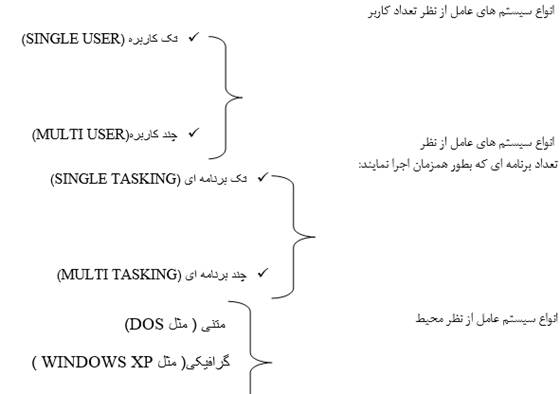
سيستم عامل DOS
تک کاربره، تک برنامه ای و متنی است.
برای اجرای فرمان موردنظر بايد دستورالعمل مربوطه را دقيقاً تايپ نمود و کليد ENTER را فشار داد، مثلاً برای مشاهده تاريخ فعلی بايد DATEرا تايپ نمود و سپس کليد ENTER را فشار داد.

شناسايي سيستم عاملWINDOWS
شرکت مايکروسافت پس از موفقيت در عرضه سيستم عامل DOS سيستم عامل تکامل يافته تری را برای کامپيوترهای شخصی ارايه داد که دارای محيط جذاب گرافيکی و کاربرپسندی بوده و با استقبال فوق العاده ای مواجه شد.
برنامه WINDOWS 3.1 ابتدا به سيستم عامل DOS متکی بوده و به آن نياز داشت. اما در سال 1995 سيستم عامل WINDOWS 95 راهی بازار شد که مستقل بوده و هيچ نيازی به سيستم عامل DOS نداشت. بعدها سيستم عاملWINDOWS 98 و سيستم عاملWINDOWS NT و سيستم عاملWINDOWS 2000 و WINDOWS ME و سيستم عامل WINDOWS XP ارايه شدند
Windows 1.0 – 1985
Windows 2.0 – 1987
Windows 3.0 – 1990
Windows 3.1 – 1992
Windows 95 – 1995
Windows 98 – 1998
Windows ME (Millennium Edition) – 2000
Windows 2000 – 2000
Windows XP – 2001
Windows Vista – 2007
Windows 7 – 2009
Windows 8 – 2012
Windows 8.1 – 2013
Windows 10 – 2015
Windows 11 – 2021
9. توانايي شناخت انتقال اطلاعات و انواع شبکه
روشهای انتقال اطلاعات(روشهای سری و موازی و ويژگيها و کاربردهای آنها)
آشنايي با تعريف شبکه کامپيوتری
آشنايي با قسمتهای اصلی يک سيستم ارتباط داده ای
(کامپيوتر فرستنده، وسيله لازم برای ارسال داده ها، کانال ارتباطی، وسيله لازم برای دريافت داده ها، کامپيوتر گيرنده)
آشنايي با انواع شبکه ها از نظر فاصله و ويژگيهای آنها
(اينترانت و اينترنت،LAN,MAN,WAN)


| قسمتهای تشکيل دهنده کامپيوتر | ||
| قسمت | توضيح | |
| Monitor (screen) صفحه نمايش | خروجی | |
| Printer چاپگر | خروجی | |
| Processor پردازنده | پردازش | |
| Keyboard صفحه کليد | ورودی | |
| Mouse ماوس | ورودی | |
| Modem مودم | Input and Output ورودی و خروجی | |
| Memory (RAM) حافظه اصلی | نگهداری موقت داده ها | |
| Floppy Disks ديسکت | نگهداری دايمی داده ها | |
| Hard Disks ديسک سخت | نگهداری دايمی داده ها | |
پرسش و پاسخ:
1- چند قطعه ودستگاه مهم سخت افزاری را نام ببريد.
پاسخ:
داخل CASE تعدادی اجزای سخت افزاری وجود دارد که با هماهنگی با نرم افزار مخصوص به سيستم کامپيوتر اجازه می دهند تا به نحو صحيح کار کند.
ROM , RAM ,CPU , motherboard, sound card,
FAX modem, hard disk drive , floppy disk drive, CD-ROM drive
2- RAM مخفف چه کلماتی است؟
Random Access Memory حافظه با دسترسي تصادفي
3- ROM مخفف چه عباراتی است؟
Read Only Memory حافظه فقط خواندني
4- CD-ROM مخفف چه کلماتی است؟
Compact Disc Read Only Memory ديسك فشرده فقط خواندني
5- واحد کيفيت خروجی چاپگر کدام است؟
dpi (dots per inch) نقطه در اينچ
در ضمن اغلب بين 300 تا 600 dpi کيفيتي مناسب می باشد.
6- واحد سرعت انتقال داده ها توسط مودم را نام ببريد.
Bps (bits per second ) بيت در ثانيه
7 – LAN مخفف چه کلماتی است؟
Local Area Network شبكه محلي
8- WAN مخفف چه کلماتی است؟
Wide Area Network شبكه گسترده
9 – ISP مخفف چه عباراتی است؟
Internet Service Provider فراهم كننده خدمات اينترنت
10- مفاهيم IT و ICT وICDL را توضيح دهيد.
IT : Information Technology فن آوري اطلاعات
ICT: Information Comunication Technology فن آوري اطلاعات و ارتباطات
ICDL: International Computer Driving licence
گواهينامه كاربری بين المللی كامپيوتر
Visual understanding: Unlocking the next frontier in AIVisual understanding: Unlocking the next frontier in AI

At the NYC AIAI Summit, Joseph Nelson, CEO & Co-Founder of Roboflow, took the stage to spotlight a critical but often overlooked frontier in AI: vision.
In a field dominated by breakthroughs in language models, Nelson argued that visual understanding – or how machines interpret the physical world – is just as essential for building intelligent systems that can operate in real-world conditions.
From powering instant replay at Wimbledon to enabling edge-based quality control in electric vehicle factories, his talk offered a grounded look at how visual AI is already transforming industries – and what it will take to make it truly robust, accessible, and ready for anything.
Roboflow now supports a million developers. Nelson walked through what some of them are building: real-world, production-level applications of visual AI across industries, open-source projects, and more. These examples show that visual understanding’s already being deployed at scale.
Three key themes in visual AI today
Nelson outlined three major points in his talk:
- The long tails of computer vision. In visual AI, long-tail edge cases are a critical constraint. These rare or unpredictable situations limit the ability of models, including large vision-language models, to fully understand the real world.
- What the future of visual models looks like. A central question is whether one model will eventually rule them all, or whether the future lies in a collection of smaller, purpose-built models. The answer will shape how machine learning is applied to visual tasks going forward.
- Running real-time visual AI at the edge. Nelson emphasized the importance of systems that run on your own data, in real-time, at the edge. This isn’t just a technical detail; it’s foundational to how visual AI will be used in the real world.
Where AI meets the real world: The role of computer vision
Joseph Nelson framed computer vision as the point where artificial intelligence intersects directly with the physical world. “At Roboflow, we think that computer vision is where AI meets the real world,” he explained.
He emphasized that vision is a primary human sense, predating even language, and pointed out that some civilizations thrived without a written system, relying instead on visual understanding. That same principle applies when building software systems: giving them vision is like giving them read access to the physical world.
This visual “read access” enables software to answer practical questions:
- How many people are in a conference room?
- Were a set of products manufactured correctly?
- Did objects make their way from point A to point B?
Nelson illustrated this with a range of real-world examples:
- Counting candies produced in a shop
- Validating traffic flows and lane usage
- Evaluating a basketball player’s shot
- Measuring field control in a soccer match
Despite the diversity of these applications, the common thread is clear: each uses visual understanding to generate actionable insights.
How Roboflow powers visual AI at scale
Roboflow’s mission is to provide the tools, platform, and solutions that enable enterprises to build and deploy visual AI. According to Nelson, users typically approach Roboflow in one of two ways:
- By creating open-source projects, much like publishing code on GitHub
- By building private projects for internal or commercial use
On the open-source front, Roboflow has become the largest community of computer vision developers on the web. The scale is significant:
- Over 500 million user-labeled and shared images
- More than 200,000 pre-trained models available
This ecosystem provides Roboflow with a unique insight into how computer vision is being applied, where it encounters challenges, and where it delivers the most value.
Roboflow also serves a wide range of enterprise customers. Nelson shared that more than half of the Fortune 100 have built with Roboflow, especially in domains grounded in the physical world, such as:
- Retail operations
- Electric vehicle manufacturing
- Product logistics and shipping
Backed by a strong network of investors, Roboflow continues to grow its platform and support the expanding needs of developers and businesses working at the intersection of AI and the real world.

Enabling the future of visual AI
Joseph Nelson outlined Roboflow’s vision for the future of visual AI: empowering developers to build models tailored to the specific scenes and contexts they care about. For this future to materialize, he emphasized two critical factors:
- Making it easy to build models that understand the right context
- Making it just as easy to deploy those models into larger systems
“When you do that,” Nelson said, “you give your software the ability to have read access to the real world.”
Open source as the backbone of progress
Roboflow’s commitment to open source is a core part of that strategy. One of their flagship open-source tools is a package called Supervision, designed to help developers process detections and masks and integrate them into broader systems.
“We’re big believers in open source AI,” Nelson explained, “as a way by which the world understands everything this technology can do.”
To illustrate adoption, he compared Supervision’s usage with that of PyTorch Vision, a widely recognized set of tools in the machine learning community. “The purple line is Supervision. The red line is PyTorch Vision. And we’re proud that some of the tools that we make are now as well recognized across the industry.”
A growing ecosystem of visual AI tools
Beyond Supervision, Roboflow maintains a suite of open-source offerings, including:
- Trackers for following objects across scenes
- Notebooks for visual understanding tasks
- Inference tools for deployment
- Maestro, a package for fine-tuning domain-specific language models (DLMs)
Together, these tools aim to simplify the entire visual AI pipeline, from training and understanding to deployment and fine-tuning, anchored in a philosophy of accessibility and openness.
The range and reality of visual AI in action
Joseph Nelson’s perspective on visual AI is grounded in scale. Roboflow has visibility into hundreds of millions of images, hundreds of thousands of datasets, and hundreds of thousands of models. This massive footprint offers deep insight into how visual AI is actually being applied in the real world.
These applications span industries and creativity levels alike, ranging from aerial understanding to pill counting in pharmaceutical settings and defect detection during product manufacturing. “And a whole host of things in between,” Nelson added.
From silly to serious: A spectrum of use cases
Roboflow, as an open-source platform, supports a wide range of users: from hobbyists working on whimsical experiments to enterprises solving mission-critical problems.
Nelson highlighted this spectrum with a few vivid examples:
- Dice roll trackers for D&D (Dungeons and Dragons): Systems that visually detect dice results during tabletop gaming sessions.
- Roof damage detection: Insurance companies use drone imagery to assess hailstorm-related roof damage.
- Vehicle production monitoring: Manufacturers inspect parts, such as those produced by stamping presses on car doors, to detect defects in real-time.
Flamethrowers and laser pointers: A creative approach
Among the more eccentric community creations:
- Flamethrower weed-killing robots. Two different developers utilized Roboflow to design robots that identify and eliminate weeds using flamethrowers. “Why pull them out,” Nelson recounted, “when I can use a flamethrower to eliminate said weeds?”
- Cat exercise machine. A developer, during COVID lockdowns, built an exercise tool for his cat by mounting a laser pointer on a robotic arm. A computer vision model tracked the cat’s position and aimed the laser ten feet away to keep the cat moving. “This one does come with a video,” Nelson joked, “and I’m sure it’s one of the most important assets you’ll get from this conference.”
These projects highlight accessibility. “A technology has really arrived,” Nelson noted, “when a hacker can take an idea and build something in an afternoon that otherwise could have seemed like a meme or a joke.”
Nelson continued with more creative and practical applications of Roboflow-powered models:
- Drone-based asset detection. Models identify swimming pools and solar panels in aerial imagery, which is useful for projects like LEED (Leadership in Energy and Environmental Design) certification that measure the renewable energy contributions to buildings.
- Zoom overlays via OBS. By integrating Roboflow with Open Broadcast Studio (OBS), users can overlay effects during video calls. For instance, specific hand gestures can trigger on-screen animations, like “Lenny,” Roboflow’s purple raccoon mascot, popping into view.
- Rickroll detection and prevention. For April Fools’ Day, the Roboflow team built a browser-based model that detects Rick Astley’s face and automatically blacks out the screen and mutes the sound, preventing the infamous “Rickroll.” This demo uses Inference JS, a library that runs models entirely client-side in the browser. It even works offline.
While playful, this approach also has commercial applications, such as content moderation, page navigation, and web agent vision for interpreting and interacting with on-page elements.
Some of Roboflow’s early inspiration came from augmented reality. Nelson shared an example of an app that uses Roboflow tools to solve AR Sudoku puzzles. Here, the front end is AR, but the back end is computer vision, which detects puzzle edges, identifies number placements, and performs a breadth-first search to solve the board.
“It’s an example of using models in production in a fun way,” Nelson said.
From demos to deployment: Roboflow in the enterprise
On the enterprise side, Roboflow supports large-scale deployment at companies like Rivian, the electric vehicle manufacturer. Over the last three years, Rivian has used Roboflow to deploy approximately 300 models into production at its Normal, Illinois, general assembly facility.
The use cases are essential to ensuring product quality:
- Verifying the correct number of screws in a battery
- Detecting bolts left on the factory floor (which can cause vehicles to jam or collide)
- Checking that paint is applied evenly and correctly
“There are hundreds and hundreds of checks that need to take place,” Nelson explained, “to ensure that a product is made correctly before it makes its way to an end user.”
Roboflow’s tools are designed not just for experimentation, but for deployment at scale. Joseph Nelson emphasized how companies like Rivian are taking advantage of this flexibility by pairing manufacturing engineers with technology teams. The result? Rapid iteration:
“I see a problem, I capture some data, I train the model, and I deploy it in an afternoon.”
This agility enables teams to solve a wide variety of small but critical manufacturing problems without waiting for long development cycles.
Self-checkout at scale: Visual AI at Walmart
Roboflow also powers instant checkout kiosks at Walmart. Describing the company playfully as an “up-and-coming retailer,” Nelson explained that Walmart’s kiosks use cameras to detect every item in a shopping cart as it enters a designated scanning zone. The system then generates a receipt automatically.
This challenge is far from trivial. Walmart stores carry hundreds of thousands of SKUs, making this a true test of model generalization and accuracy in real-world conditions. Despite the complexity, Nelson noted with pride that these systems have made it into production at multiple locations, with photo evidence to prove it.
Instant replay at major tennis events
Another high-profile deployment: instant replay at Wimbledon, the US Open, and the French Open (Roland Garros). Roboflow’s computer vision models are used to:
- Detect the positions of tennis players and the ball
- Map out the court in real time
- Enable automated camera control and clip selection for ESPN+ replays
This use case reinforces the versatility of visual AI. Nelson even drew a humorous parallel:
“Remember that cat workout machine? Turns out it’s actually not so different from the same things that people enjoy at one of the world’s most popular tennis events.”
From hacks to healthcare: More unconventional use cases
Nelson wrapped this section with two more examples that demonstrate visual AI’s creative range, from civic life to scientific research.
- Tennis court availability alerts. A hacker in San Francisco set up a camera on his windowsill to monitor public tennis courts. Using a custom-trained model, the system detects when the court is empty and sends him a text, so he can be the first to play.
- Accelerating cancer research. At a university in the Netherlands, researchers are using computer vision to count neutrophils, a protein reaction observed after lab experiments. Previously, this required manual analysis by graduate students. Now, automation speeds up the review process, allowing faster iteration and contributing, albeit in a small way, to accelerating treatments for critical diseases.
What comes next for visual AI?
With a wide array of applications, ranging from retail to robotics to research, visual AI is already shaping various industries. As Joseph Nelson transitioned to the next part of his talk, he posed the central question:
“So what gives? What’s the holdup? What happens next, and where is the field going?”
That’s the conversation he takes on next.
As visual AI moves from research labs into production, it must contend with the messy, unpredictable nature of the real world. Joseph Nelson explained this challenge using a familiar concept: the normal distribution.
When it comes to visual tasks, the distribution is far from tidy. While some common categories, like people, vehicles, and food, fall within the high-density “center” of the curve (what Nelson calls “photos you might find on Instagram”), there’s a very long tail of edge cases that AI systems must also learn to handle.
These long tails include:
- Hundreds of thousands of unique SKUs in retail environments like Walmart
- Novel parts are produced in advanced manufacturing settings like Rivian’s facilities
- Variable lighting conditions for something as niche as solving a Sudoku puzzle

Why visual data is uniquely complex
Nelson also emphasized a fundamental difference between visual and textual data: density and variability. While all of the text can be encoded compactly in Unicode, even a single image contains vastly more data, with RGB channels, lighting nuances, textures, and perspective all influencing interpretation.
“From a very first principles view, you can see that the amount of richness and context to understand in the visual world is vast.”
Because of this complexity, fully reliable zero-shot or multi-shot performance in visual AI remains aspirational. To achieve dependable results, teams must often rely on:
- Multi-turn prompting
- Fine-tuning
- Domain adaptation
Put simply, Nelson said, “The real world’s messy.”
When small errors become big problems
The stakes for accuracy grow when visual AI is used in regulated or high-risk environments. Nelson shared an example from a telepharmacy customer using Roboflow to count pills.
This customer is accountable to regulators for correctly administering scheduled substances. A count that’s off by just one or two pills per batch may seem minor, but when that error scales across all patients, it creates major discrepancies in inventory.
Worse, Nelson noted a surprising discovery: telepharmacists with painted long nails occasionally caused the model to misclassify fingers as pills. This kind of visual anomaly wouldn’t appear in a clean training dataset, but it’s common in real-world deployments.
This example illustrates a critical principle in visual AI:
Real-world reliability requires robust systems trained on representative data and a readiness for edge cases that defy textbook distributions.
Why existing datasets aren’t enough
Joseph Nelson pointed to a key limitation in visual AI: many models are trained and evaluated on narrow, conventional datasets that don’t reflect the full diversity of the real world.
A common reference point is the COCO (Common Objects in Context) dataset, created by Microsoft between 2012 and 2014. It includes 80 familiar classes such as person, food, and dog. Nelson described this as data that falls “right up the center of the bell curve.”
But the world is far messier than that. To push the field forward, Nelson argued, we need more than common object detection; we need better evaluation frameworks that test whether models can adapt to novel domains.
Introducing RF100VL: A new benchmark for visual AI
To address this, Roboflow introduced RF100VL, short for Roboflow 100 Vision Language. While the name may not be flashy, the purpose is clear: provide a more accurate view of model performance in the real world.
RF100VL consists of:
- 100 datasets
- 100,000 images
- Covering diverse domains, such as:
- Microscopic and telescopic imagery
- Underwater environments
- Document analysis
- Digital worlds
- Industrial, medical, aerial, and sports contexts
- Flora and fauna categories
This dataset reflects how developers and companies are actually using computer vision. Because Roboflow hosts the largest community of computer vision developers, RF100VL is built from real-world production data and maintained by the community itself.
“If COCO is a measurement of things you would commonly see,” Nelson said, “RF100VL is an evaluation of everything else, the messy parts of the real world.”
Testing zero-shot performance
Nelson highlighted the limitations of current models by sharing evaluation results. For example, the best-performing zero-shot model on RF100VL (Grounding DINO) achieved just 15.7% accuracy. That’s with no fine-tuning, meant to simulate a model’s raw ability to generalize across unseen tasks.
“Even the best models in the world today still lack the ability to do what’s called grounding and understanding of relatively basic things.”
RF100VL aims to fill that gap. It allows developers to hold large models accountable and measure whether they generalize well across domains.
Scaling like language models
So how can we improve visual understanding? Nelson pointed to the same approach used in language AI:
- Pre-training at a large scale
- Expanding datasets to include the long tail
- Providing rich, diverse context for model adaptation
In the same way large language models improved through massive, inclusive training sets, visual AI must follow suit. Nelson emphasized that context is king in this process.
Tools for diagnosing model gaps
To make evaluation accessible, Roboflow launched visioncheckup.com, a playful but practical tool for visual model assessment. “It’s like taking your LLM to the optometrist,” Nelson said. The site simulates a vision test, showing where a model struggles and where it succeeds.
While some visual tasks, such as counting or visual question answering, still trip up models, Nelson noted that progress is accelerating. And he made his bet clear:
“I would bet on the future of open science.”
Why real-time performance at the edge matters
As the talk turned toward deployment, Nelson highlighted one major difference between language and vision models: where and how they run.
Language tasks often benefit from:
- Cloud hosting
- Access to extensive compute resources
- Room for delayed, test-time reasoning (e.g., web lookups)
But visual systems frequently need to operate:
- In real time
- On edge devices
- With no reliance on cloud latency or large compute pools
“Models need to run fast, real time, and often at the edge,” Nelson said.
This makes deployment requirements for visual AI fundamentally different and much more constrained than those for language-based systems.
Why edge performance matters
Joseph Nelson closed his talk by returning to a central constraint in visual AI: latency.
Unlike many language-based AI tasks, visual systems often have to operate under real-time conditions, especially in settings like live sports broadcasts. For example, Wimbledon doesn’t have the luxury of cloud processing, even with high-speed internet. Every frame must be processed live, with sub–10 millisecond latency.
This creates a pressing requirement: models that run efficiently on constrained hardware, without sacrificing accuracy.
“You need to have models that can perform in edge conditions… on smaller or constrained compute and run in real time.”
Edge deployment isn’t just for industrial hardware, like NVIDIA Jetsons. Nelson highlighted another vision: empowering individual developers to run models on their own machines, locally and independently.
“We can actually kind of power the rebels so that anyone can create, deploy, and build these systems.”
Introducing RF-DETR: Transformers at the edge
To address the challenge of bringing large-model performance to real-time use cases, Roboflow developed RF-DETR, short for Roboflow Detection Transformer. This model is designed to combine the contextual strength of transformers with the speed and deployability needed at the edge.
Nelson contrasted it with existing models, like the YOLO family, which are built around CNNs and optimized for speed. RF-DETR aims to bring the pre-training depth of transformers into the real-time performance zone.
“How do we take a large transformer and make it run in real time? That’s what we did.”
RF-DETR was benchmarked on both:
- Microsoft COC for conventional object detection
- RF100VL to measure real-world adaptability

Bridging the gap to visual AGI
In wrapping up, Nelson tied together the major themes of his talk:
- Better datasets (like RF100VL)
- Better models (like RF-DETR)
- Deployment flexibility, including on constrained and local hardware
Together, these advancements move us beyond the metaphor of “a brain in a jar.” Instead, Nelson described the vision for a true visual cortex, a key step toward real-world AI systems that can see, reason, and act.
“When we build with Roboflow… you’re a part of making sure that AI meets the real world and delivers on the promise of what we know is possible.”
Final thoughts
Joseph Nelson closed his talk at the NYC AIAI Summit with a clear message: for AI to meet the real world, it must see and understand it. That means building better datasets, such as RF100VL, creating models that generalize across messy, real-world domains, and ensuring those models can run in real-time, often at the edge.
From live sports broadcasts to pharmaceutical safety checks, and from open-source cat toys to advanced vehicle assembly lines, the breadth of visual AI’s impact is already vast. But the work is far from over. As Nelson put it, we’re still crossing the bridge, from large models as “brains in a jar” to intelligent systems with a working visual cortex.
By contributing to open-source tools, adapting models for deployment in the wild, and holding systems accountable through realistic evaluations, developers and researchers alike play a crucial role in advancing visual understanding. Roboflow’s mission is to support that effort, so that AI not only thinks, but sees.
How Agentic AI is transforming healthcare deliveryHow Agentic AI is transforming healthcare delivery

In the Agents of Change podcast, host Anthony Witherspoon welcomes Archie Mayani, Chief Product Officer at GHX (Global Healthcare Exchange), to explore the vital role of artificial intelligence (AI) in healthcare.
GHX is a company that may not be visible to the average patient, but it plays a foundational role in ensuring healthcare systems operate efficiently. As Mayani describes it, GHX acts as “an invisible operating layer that helps hospitals get the right product at the right time, and most importantly, at the right cost.”
GHX’s mission is bold and clear: to enable affordable, quality healthcare for all. While the work may seem unglamorous, focused on infrastructure beneath the surface, it is, in Mayani’s words, “mission critical” to the healthcare system.
Pioneering AI in the healthcare supply chain
AI has always been integral to GHX’s operations, even before the term became a buzzword. Mayani points out that the company was one of the early adopters of technologies like Optical Character Recognition (OCR) within healthcare supply chains, long before such tools were formally labeled as AI.
This historical context underlines GHX’s longstanding commitment to innovation.
Now, with the rise of generative AI and agentic systems, the company’s use of AI has evolved significantly. These advancements are being harnessed for:
- Predicting medical supply shortages
- Enhancing contract negotiations for health systems
- Improving communication between clinicians and supply chain teams using natural language interfaces
All of these tools are deployed in service of one goal: to provide value-based outcomes and affordable care to patients, especially where it’s needed most.
Building resilience into healthcare with “Resiliency AI”
GHX builds resilience. That’s the ethos behind their proprietary system, aptly named Resiliency AI. The technology isn’t just about automation or cost-savings; it’s about fortifying healthcare infrastructure so it can adapt and thrive in the face of change.
Mayani articulates this vision succinctly: “We are not just building tech for healthcare… we are building resilience into healthcare.”
Anthony, the podcast host, highlights a key point: AI’s impact in healthcare reaches far beyond business efficiency. It touches lives during their most vulnerable moments.
The episode highlights a refreshing narrative about AI: one not focused on threats or ethical concerns, but rather on how AI can be an instrument of positive, human-centered change.
The imperative of responsible AI in healthcare
One of the core themes explored in this episode of Agents of Change is the pressing importance of responsible AI; a topic gaining traction across industries, but particularly crucial in healthcare. Host Anthony sets the stage by highlighting how ethics and responsibility are non-negotiable in sectors where human lives are at stake.
Archie Mayani agrees wholeheartedly, emphasizing that in healthcare, the stakes for AI development are dramatically different compared to other industries. “If you’re building a dating app, a hallucination is a funny story,” Mayani quips. “But in [healthcare], it’s a lawsuit; or worse, a life lost.” His candid contrast underscores the life-critical nature of responsible AI design in the medical field.

Transparency and grounding: The foundation of ethical AI
For GHX, building responsible AI begins with transparency and grounding. Mayani stresses that these principles are not abstract ideals, but operational necessities.
“Responsible AI isn’t optional in healthcare,” he states. It’s embedded in how GHX trains its AI models, especially those designed to predict the on-time delivery of surgical supplies, which are crucial for patient outcomes.
To ensure the highest level of reliability, GHX’s AI models are trained on a diverse range of data:
- Trading partner data from providers
- Fulfillment records
- Supplier reliability statistics
- Logistical delay metrics
- Historical data from natural disasters
This comprehensive data approach allows GHX to build systems that not only optimize supply chain logistics but also anticipate and mitigate real-world disruptions, delivering tangible value to hospitals and, ultimately, patients.
Explainability is key: AI must justify its decisions like a clinician
One of the most compelling points Archie Mayani makes in the discussion is that AI must explain its logic with the clarity and accountability of a trained clinician. This is especially important when dealing with life-critical healthcare decisions. At GHX, every disruption prediction produced by their AI system is accompanied by a confidence score, a criticality ranking, and a clear trace of the data sources behind the insight.
“If you can’t explain it like a good clinician would, your AI model is not going to be as optimized or effective.”
This standard of explainability is what sets high-functioning healthcare AI apart. It’s not enough for a model to provide an output; it must articulate the “why” behind it in a way that builds trust and enables action from healthcare professionals.
Avoiding AI hallucinations in healthcare
Mayani also reflects on historical missteps in healthcare AI to highlight the importance of data diversity and governance. One case he references is early AI models for mammogram interpretation. These systems produced unreliable predictions because the training data lacked diversity across race, ethnicity, and socioeconomic background.
This led to models that “hallucinated”, not in the sense of whimsical errors, but with serious real-world implications. For example, differences in breast tissue density between African American and Caucasian women weren’t properly accounted for, leading to flawed diagnostic predictions.
To counteract this, GHX emphasizes:
- Inclusive training datasets across demographic and physiological variables
- Rigorous data governance frameworks
- A learning mindset that adapts models based on real-world feedback and outcomes
This commitment helps ensure AI tools in healthcare are equitable, reliable, and aligned with patient realities, not just technical possibilities.
The conversation also touches on a universal truth in AI development: the outputs of any model are only as good as the inputs provided. As Anthony notes, AI doesn’t absolve humans of accountability. Instead, it reflects our biases and decisions.
“If an AI model has bias, often it’s reflective of our own societal bias. You can’t blame the model; it’s showing something about us.”
This reinforces a central thesis of the episode: Responsible AI begins with responsible humans; those who train, test, and deploy the models with intention, transparency, and care.
Earning confidence in AI-driven healthcare
As AI becomes more embedded in healthcare, public fear and discomfort are natural reactions, particularly when it comes to technologies that influence life-altering decisions. Anthony captures this sentiment, noting that any major innovation, especially in sensitive sectors like healthcare, inevitably raises concerns.
Archie Mayani agrees, emphasizing that fear can serve a constructive purpose. “You’re going to scale these agents and AI platforms to millions and billions of users,” he notes. “You better be sure about what you’re putting out there.” That fear, he adds, should drive greater diligence, bias mitigation, and responsibility in deployment.
The key to overcoming this fear? Transparency, communication, and a demonstrable commitment to ethical design. As Mayani and Anthony suggest, trust must be earned, not assumed. Building that trust involves both technical rigor and emotional intelligence to show stakeholders that AI can be both safe and valuable.
The challenge of scaling agentic AI in healthcare
With a strong foundation in ethical responsibility, the conversation shifts to a pressing concern: scaling agentic AI models in healthcare environments. These are AI systems capable of autonomous decision-making within predefined constraints, highly useful, but difficult to deploy consistently at scale.
Mayani draws an apt analogy: scaling agentic AI in healthcare is like introducing a new surgical technique.
“You have to prove it works, and then prove it works everywhere.”
This speaks to a fundamental truth in health tech: context matters. An AI model trained on datasets from the Mayo Clinic, for example, cannot be transplanted wholesale into a rural community hospital in Arkansas. The operational environments, patient demographics, staff workflows, and infrastructure are vastly different.
Key barriers to AI scalability in healthcare
- Contextual variability. Every healthcare setting is unique in terms of needs, infrastructure, and patient populations.
- Data localization. Models must be fine-tuned to reflect local realities, not just generalized benchmarks.
- Performance assurance. At scale, AI must remain accurate, explainable, and effective across all points of care.
For product leaders like Mayani, scale and monetization are the twin pressures of modern AI deployment. And in healthcare, the cost of getting it wrong is too high to ignore.
GHX’s resiliency center: A scalable AI solution in action
To illustrate how agentic AI can be successfully scaled in healthcare, Archie Mayani introduces one of GHX’s flagship products: Resiliency Center. This tool exemplifies how AI can predict and respond to supply chain disruptions at scale, offering evidence-based solutions in real time.
Resiliency Center is designed to:
- Accurately categorize and predict potential disruptions in the healthcare supply chain
- Recommend clinical product alternatives during those disruptions
- Integrate seamlessly across dozens of ERP systems, even with catalog mismatches
- Provide evidence-backed substitute products, such as alternatives to specific gloves or catheters likely to be back-ordered
These “near-neighborhood” product recommendations are not only clinically valid, but context-aware. This ensures that providers always have access to the right product, at the right time, at the right cost, a guiding principle for GHX.
“The definition of ‘right’ is really rooted in quality outcomes for the patient and providing access to affordable care, everywhere.”
This operational model is a clear example of scaling with purpose. It reflects Mayani’s earlier point: you can’t scale effectively without training on the right datasets and incorporating robust feedback loops to detect and resolve model inaccuracies.
Making sense of healthcare data
As the conversation shifts to the nature of healthcare data, Anthony raises a key issue: data fragmentation. In healthcare, data often exists in disconnected silos, across hospitals, systems, devices, and patient records, making it notoriously difficult to use at scale.
Mayani affirms that overcoming this fragmentation is essential for responsible and effective AI. The foundation of scalable, bias-free, and high-performance AI models lies in two critical pillars:
- Data diversity. AI systems must be trained on varied and inclusive datasets that reflect different patient populations, healthcare contexts, and operational environments.
- Data governance. There must be strict protocols in place to manage, verify, and ethically handle healthcare data. This includes everything from ensuring data integrity to setting up feedback mechanisms that refine models over time.
“All of that, scaling, performance, bias mitigation, it ultimately comes down to the diversity and governance of the data.”
This framing offers a critical insight for healthcare leaders and AI practitioners alike: data is the bedrock of trustworthy AI systems in medicine.

Why local context and diverse data matter in healthcare AI
One of the most illustrative examples of data diversity’s value came when GHX’s models flagged a surgical glove shortage in small rural hospitals, a disruption that wasn’t immediately visible in larger healthcare systems. Why?
- Rural hospitals often have different reorder thresholds.
- They typically lack buffer stock and have fewer supplier relationships compared to large Integrated Delivery Networks (IDNs).
This nuanced insight could only emerge from a truly diverse dataset. As Archie Mayani explains, if GHX had only trained its models using data from California, it might have overlooked entirely seasonal and regional challenges, like hurricanes in the Southeast or snowstorms in Minnesota, that affect supply chains differently.
“Healthcare isn’t a monolith. It’s a mosaic.”
That mosaic requires regionally relevant, context-sensitive data inputs to train agentic AI systems capable of functioning across a broad landscape of clinical settings.
Trust and data credibility: The often overlooked ingredient
Diversity in data is only part of the solution. Trust in data sources is equally critical. Archie points out a fundamental truth: not all datasets are equally valid. Some may be outdated, siloed, or disconnected from today’s realities. And when AI systems train on these flawed sources, their predictions suffer.
This is where GHX’s role as a trusted intermediary becomes essential. For over 25 years, GHX has served as a neutral and credible bridge between providers and suppliers, earning the trust required to curate, unify, and validate critical healthcare data.
“You need a trusted entity… not only for diverse datasets, but the most accurate, most reliable, most trusted datasets in the world.”
GHX facilitates cooperation across the entire healthcare data ecosystem, including:
- Hospitals and providers
- Medical suppliers and manufacturers
- Electronic Medical Record (EMR) systems
- Enterprise Resource Planning (ERP) platforms
This integrated ecosystem approach ensures the veracity of data and enables more accurate, bias-aware AI models.
Diversity and veracity: A dual mandate for scalable AI
Anthony aptly summarizes this insight as a two-pronged strategy: it’s not enough to have diverse datasets; you also need high-veracity data that’s trusted, updated, and contextually relevant. Mayani agrees, adding that agentic AI cannot function in isolation; it depends on a unified and collaborative network of stakeholders.
“It’s beyond a network. It’s an ecosystem.”
By connecting with EMRs, ERPs, and every link in the healthcare chain, GHX ensures its AI models are both informed by real-world variability and grounded in validated data sources.
From classical AI to agentic AI: A new era in healthcare
Archie Mayani makes an important distinction between classical AI and agentic AI in healthcare. For decades, classical AI and machine learning have supported clinical decision-making, especially in diagnostics and risk stratification. These systems helped:
- Identify patients with complex comorbidities
- Prioritize care for those most at risk
- Power early diagnostic tools such as mammography screenings
“We’ve always leveraged classical AI in healthcare… but agentic AI is different.”
Unlike classical models that deliver discrete outputs, agentic AI focuses on workflows. It has the potential to abstract, automate, and optimize full processes, making it uniquely suited to address the growing pressures in modern healthcare.
Solving systemic challenges with agentic AI
Mayani highlights the crisis of capacity in today’s healthcare systems, particularly in the U.S.:
- Staff shortages across both clinical and back-office roles
- Rising operational costs
- Fewer trained physicians are available on the floor
In this context, agentic AI emerges as a co-pilot. It supports overburdened staff by automating routine tasks, connecting data points, and offering intelligent recommendations that extend beyond the exam room.
One of the most compelling examples Mayani shares involves a patient with recurring asthma arriving at the emergency department. Traditionally, treatment would focus on the immediate clinical issue. But agentic AI can see the bigger picture:
- It identifies that the patient lives near a pollution site
- Notes missed follow-ups due to lack of transportation
- Recognizes socioeconomic factors contributing to the recurring condition
With this information, the healthcare team can address the root cause, not just the symptom. This turns reactive treatment into proactive, preventative care, reducing waste and improving outcomes.
“Now you’re not treating a condition. You’re addressing a root cause.”
This approach is rooted in the Whole Person Care model, which Mayani recalls from his earlier career. While that model once relied on community health workers stitching together fragmented records, today’s agentic AI can do the same work; faster, more reliably, and at scale.
Agentic AI as a member of the care team
Ultimately, Mayani envisions agentic AI as a full-fledged member of the care team, one capable of:
- Intervening earlier in a patient’s health journey
- Coordinating care across departments and disciplines
- Understanding and integrating the social determinants of health
- Delivering on the promise of Whole Person Care
This marks a paradigm shift, from episodic, condition-focused care to integrated, data-driven, human-centered healing.
One of the most transformative promises of agentic AI in healthcare is its ability to identify root causes faster, significantly reducing both costs and systemic waste. As Anthony notes, the delay in getting to a solution often drives up costs unnecessarily, and Mayani agrees.
“Prevention is better than cure… and right now, as we are fighting costs and waste, it hasn’t been truer than any other time before.”
Agentic AI enables care teams to move from reactive service delivery to proactive problem-solving, aligning healthcare with long-promised, but rarely achieved, goals like holistic and whole-person care. The way Mayani describes it, this is now a practical, scalable reality.
COVID-19: A catalyst for AI innovation in supply chain resilience
Looking back at the COVID-19 pandemic, Mayani reflects on one of the biggest shocks to modern healthcare: supply chain collapse. It wasn’t due to a lack of data; healthcare generates 4x more data than most industries. The failure was one of foresight and preparedness.
“The supply chain broke not because we didn’t have the data, but because we didn’t have the foresight.”
This crisis has become a compelling event that has accelerated innovation. GHX’s own AI-driven Resiliency Center now includes early versions of systems that can:
- Detect high-risk items like ventilator filters at risk of shortage
- Recommend five clinically approved alternatives, sorted by cost, delivery time, and supplier reliability
- Provide real-time, evidence-based recommendations across a multi-stakeholder ecosystem
Mayani likens this transformation to going from a smoke detector to a sprinkler system; not just identifying the problem, but acting swiftly to stop it before it spreads.

Learning from crisis: Building a proactive future
COVID-19 may have been an unprecedented tragedy, but it forced healthcare organizations to centralize data, embrace cloud infrastructure, and accelerate digital transformation.
Before 2020, many health systems were still debating whether mission-critical platforms should move to the cloud. Post-crisis, the conversation shifted from adoption to acceleration, opening the door to advanced technologies like AI and GenAI.
“Necessity leads to innovation,” as Anthony puts it, and Mayani agrees.
The result is a more resilient, more responsive healthcare system, better equipped to navigate future challenges, from pandemics to geopolitical shifts to tariff policy changes. GHX now plays a pivotal role in helping suppliers and providers understand and act on these evolving variables through data visibility and decision-making intelligence.
AI hallucinations in healthcare
While agentic AI offers powerful capabilities, hallucinations remain a significant risk, particularly in healthcare, where errors can have devastating consequences. Archie Mayani openly acknowledges this challenge: even with high-quality, diverse, and rigorously governed datasets, hallucinations can still occur.
Drawing from his early work with diagnostic models for lung nodules and breast cancer detection, Mayani explains that hallucinations often stem from data density issues or incomplete contextual awareness. These can lead to outcomes like:
- Recommending a nonexistent or back-ordered medical supply erodes trust
- Incorrectly suggesting a serious diagnosis, such as early breast cancer, to a healthy individual
Both are catastrophic in their own way, and both highlight the need for fail-safes and human oversight.
GHX’s guardrails against AI errors
To mitigate these risks, GHX employs a multi-layered approach:
- Validated data only. Models pull from active, verified medical supply catalogs.
- Human-in-the-loop systems. AI makes predictions, but a human still approves the final decision.
- Shadow mode training. New models run in parallel with human-led processes until they reach high reliability.
- “Residency training” analogy. Mayani likens early AI models to junior doctors under supervision; they’re not allowed to operate independently until they’ve proven their accuracy.
This framework ensures that AI earns trust through performance, reliability, and responsibility, not just promises.
The future of agentic AI
When asked to predict the future of agentic AI in healthcare, Mayani presents a powerful vision: a world where AI becomes invisible.
“When AI disappears… that’s when we’ve truly won.”
He envisions a future where AI agents across systems, such as GHX’s Resiliency AI and hospital EMRs, communicate autonomously. A nurse, for instance, receives necessary supplies without ever placing an order, because the agents already anticipated the need based on scheduled procedures and clinical preferences.
Indicators of AI maturity
- Care is coordinated automatically without juggling apps or administrative steps.
- Agentic AI enables seamless, behind-the-scenes action, optimizing outcomes while removing friction.
- Patients receive timely, affordable, personalized care, not because someone made a phone call, but because the system understood and acted.
This is the true potential of agentic AI: not to dazzle us with flashy features, but to blend so naturally into the work that it disappears.
The normalization of AI
As AI becomes more embedded in daily life, public perception is shifting from fear to discovery, and now, toward normalization. As Mayani and Anthony discuss, many people already use AI daily (in smartphones, reminders, and apps) without even realizing it.
The goal is for agentic AI to follow the same path: to support people, not replace them; to augment creativity, not suppress it; and to enable higher-order problem-solving by removing repetitive, predictable tasks.
“It’s never about the agents taking over the world. They are here so that we can do the higher-order bits.”
The path forward for Agentic AI in healthcare
The future of healthcare lies not in whether AI will be used but how. And leaders like Archie Mayani at GHX are laying the foundation for AI that is ethical, explainable, resilient, and invisible.
From predicting disruptions and recommending evidence-based alternatives to coordinating care and addressing root causes, agentic AI is already reshaping how we deliver and experience healthcare.
The next chapter is about when it quietly steps into the background, empowering humans to do what they do best: care.

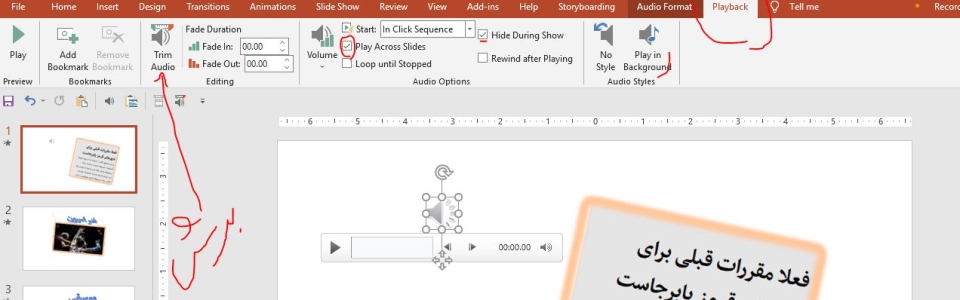
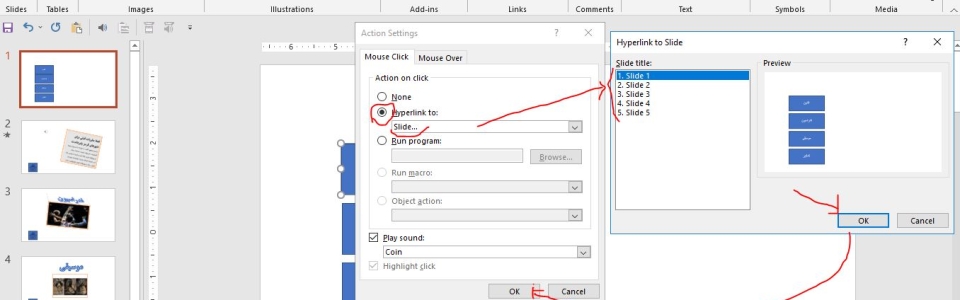
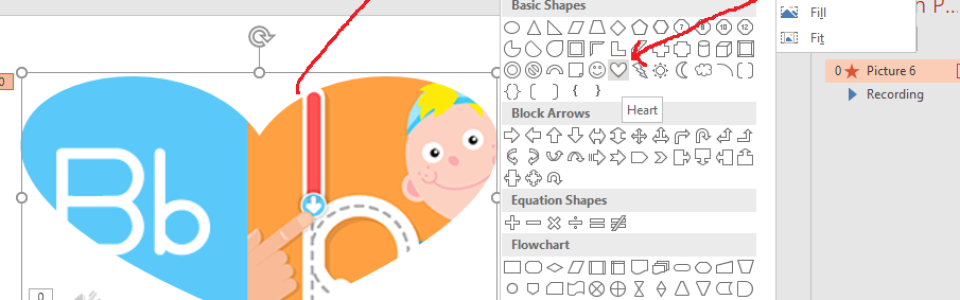

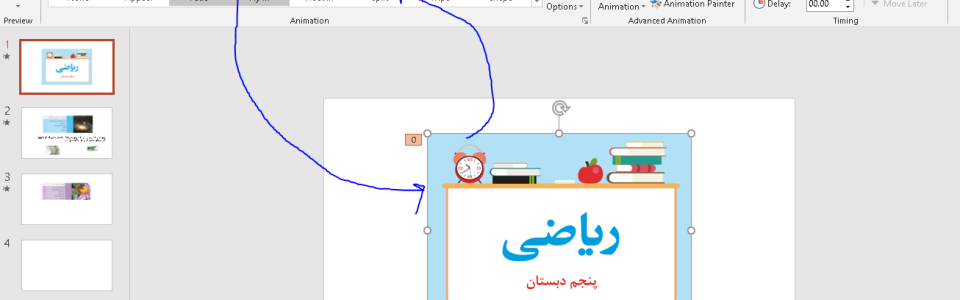
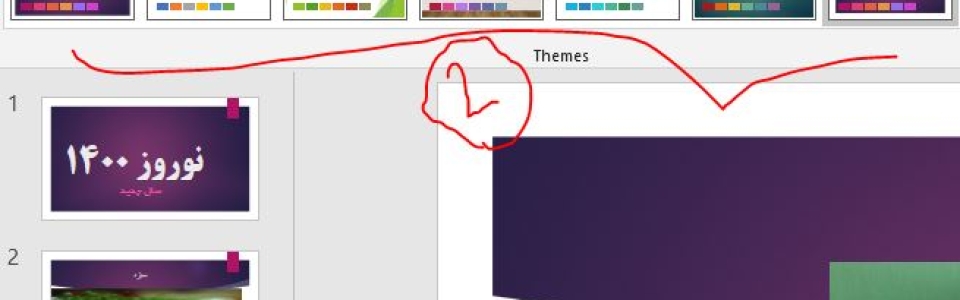
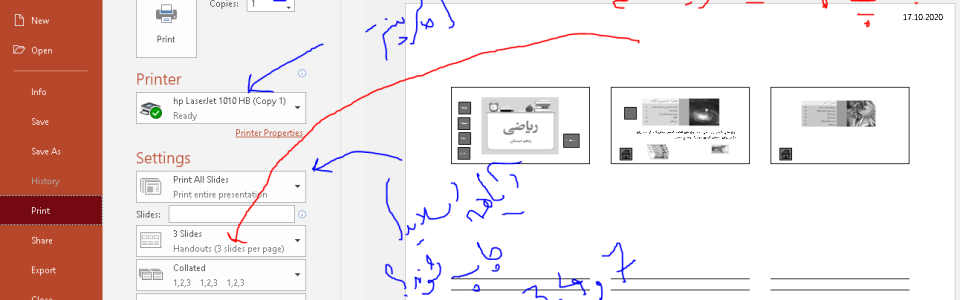
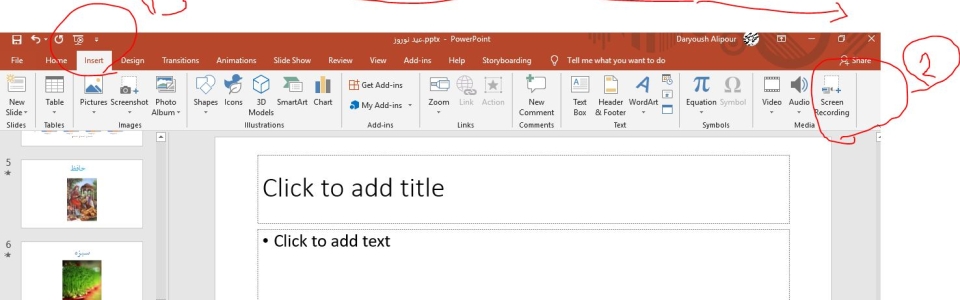
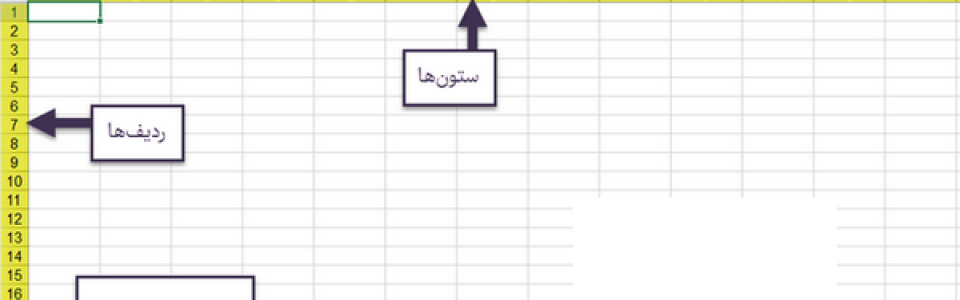
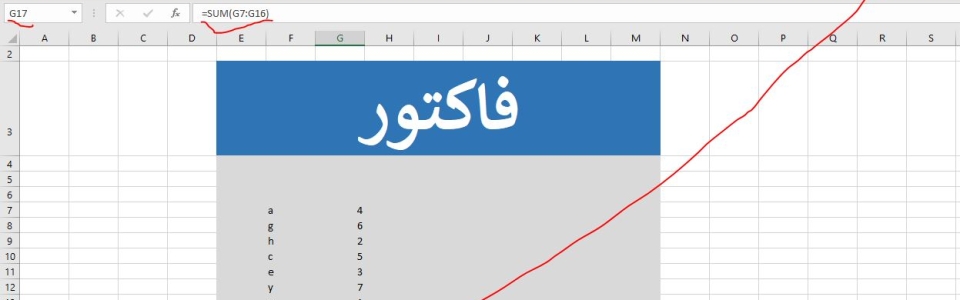
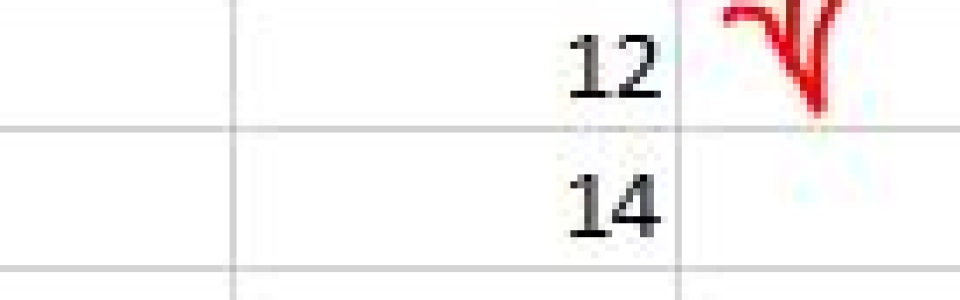
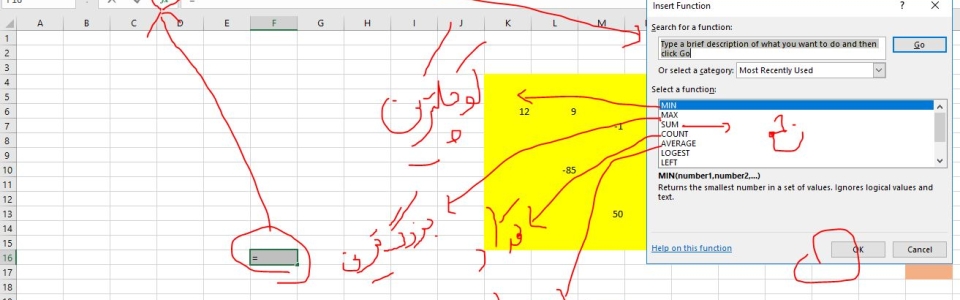
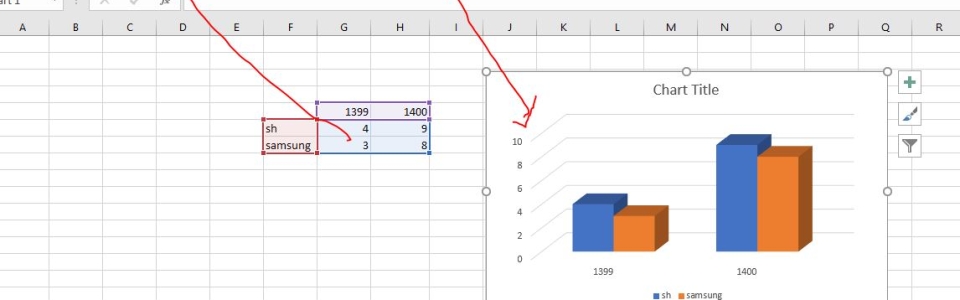
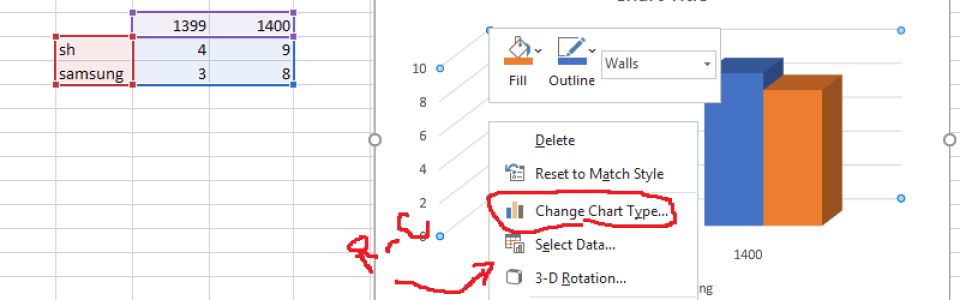
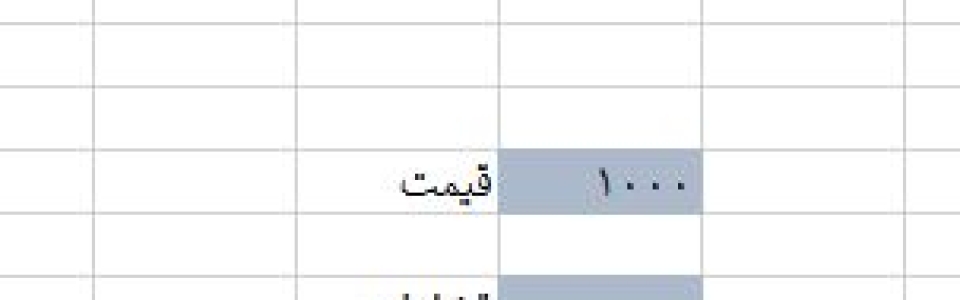
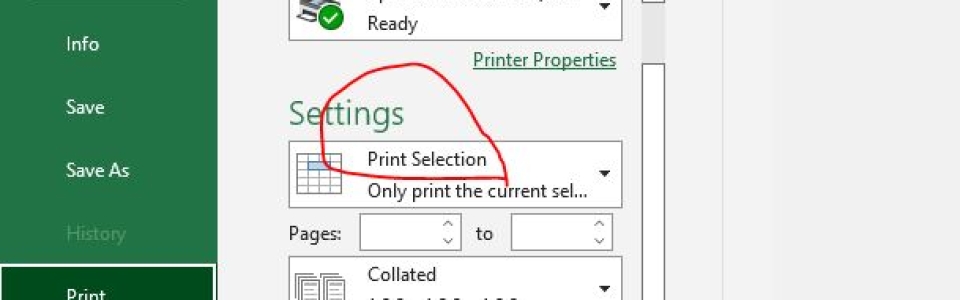
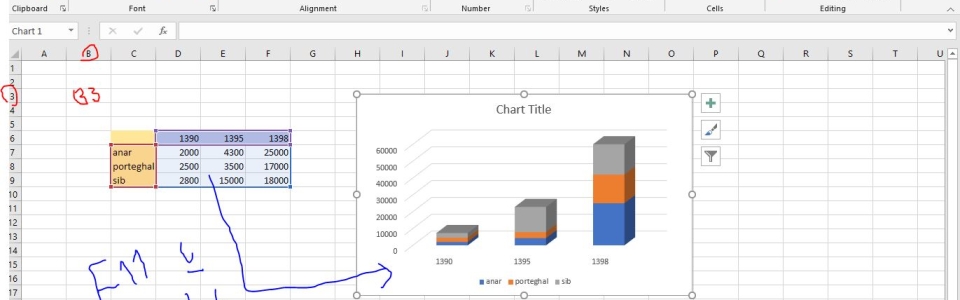
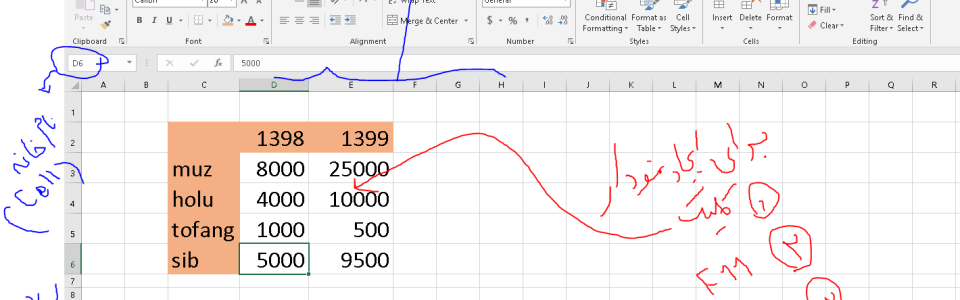
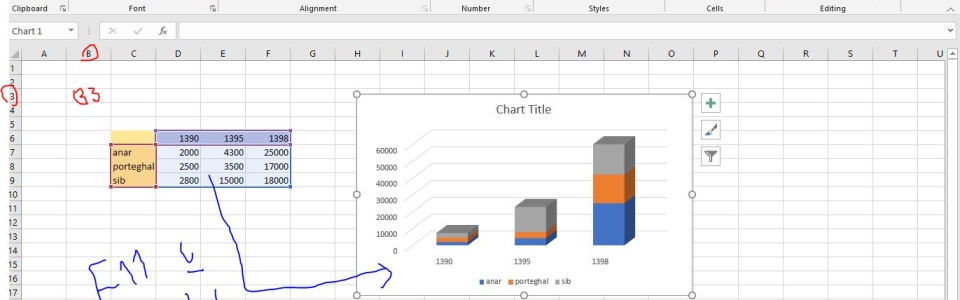
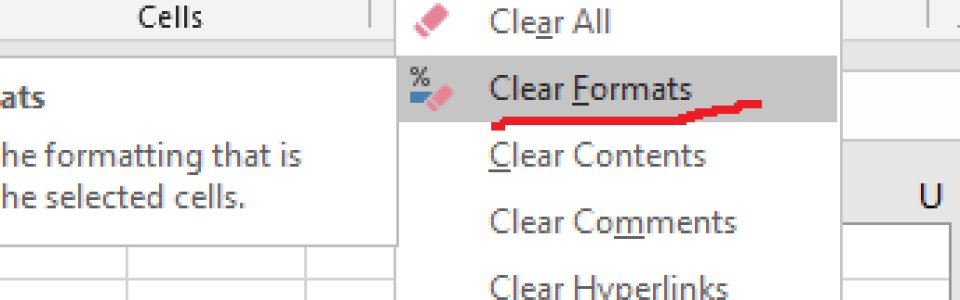
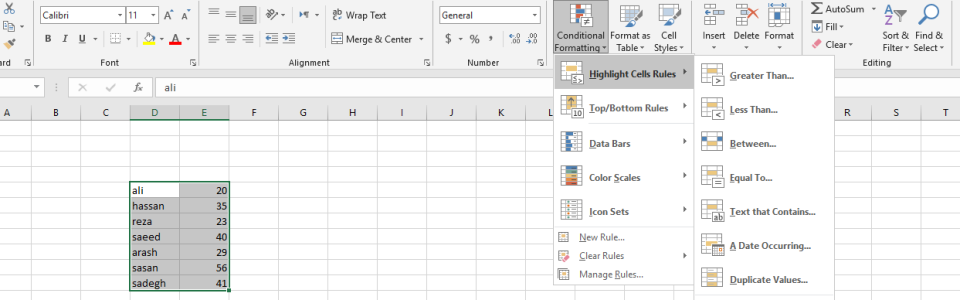
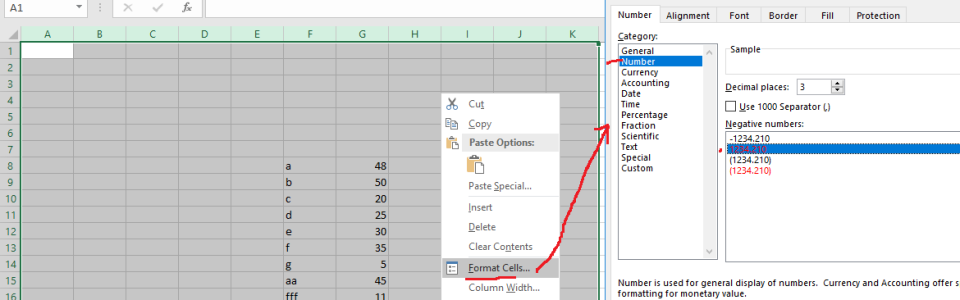
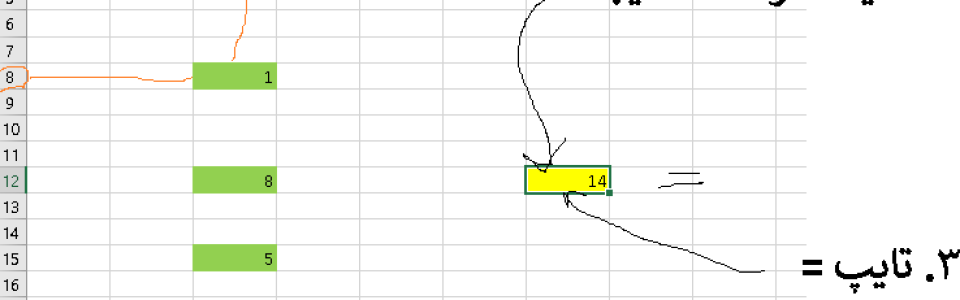
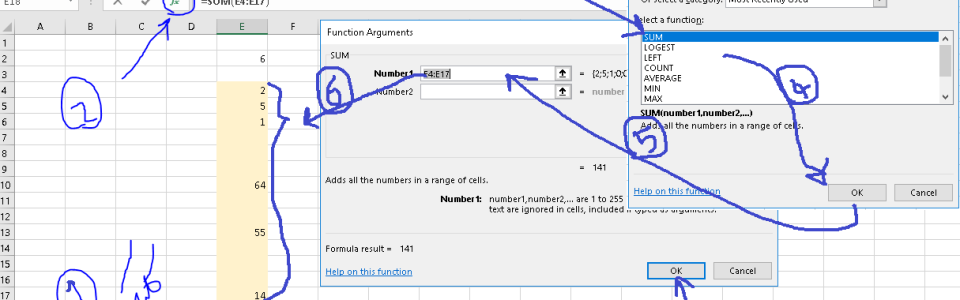
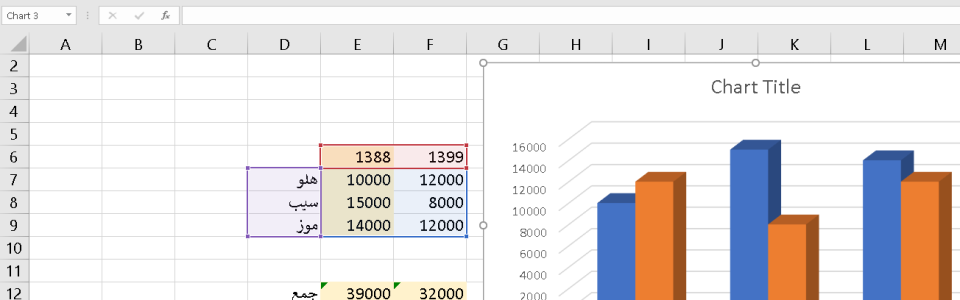

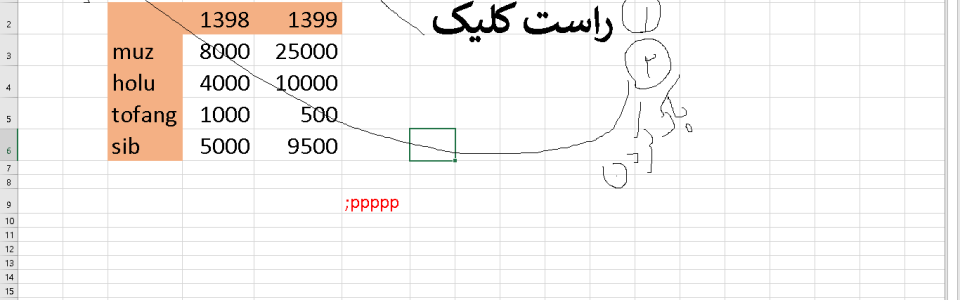
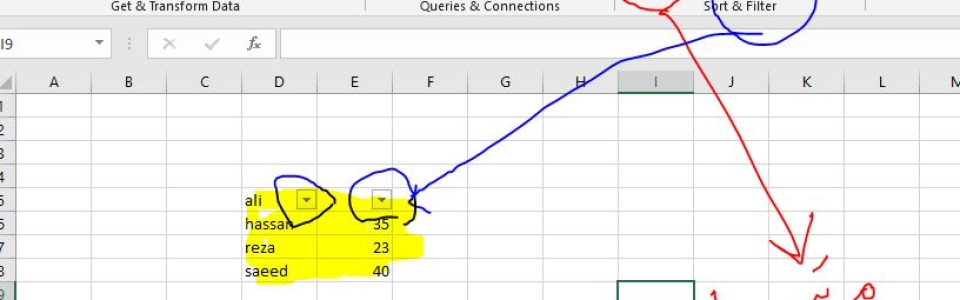
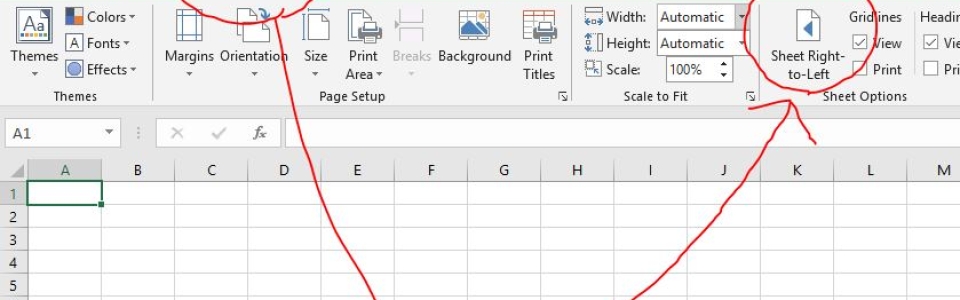
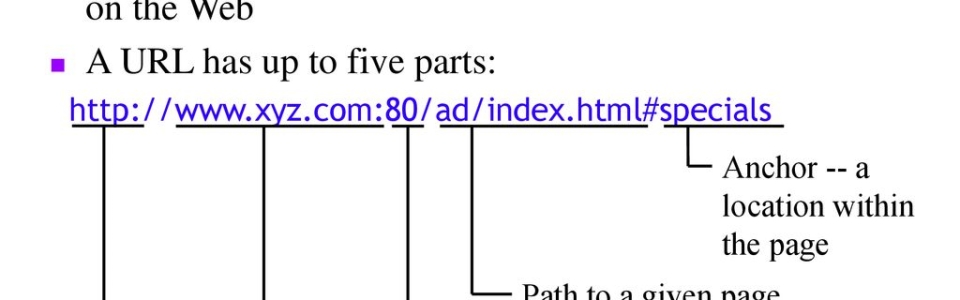


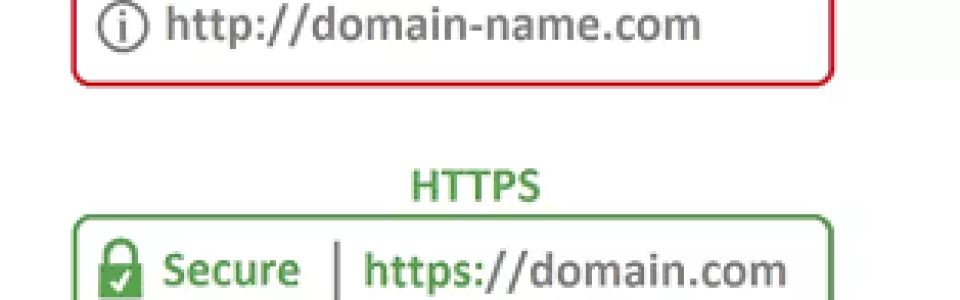
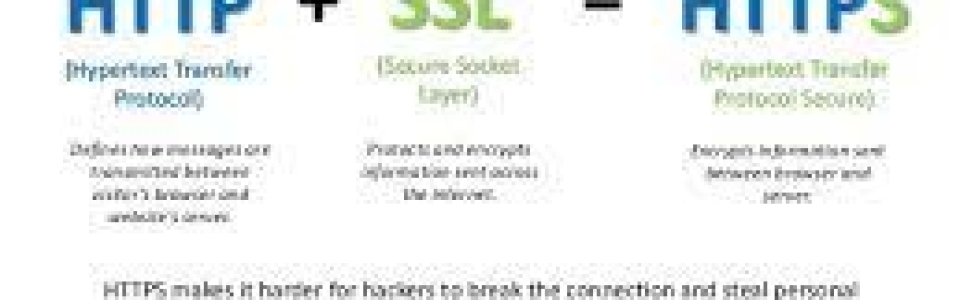
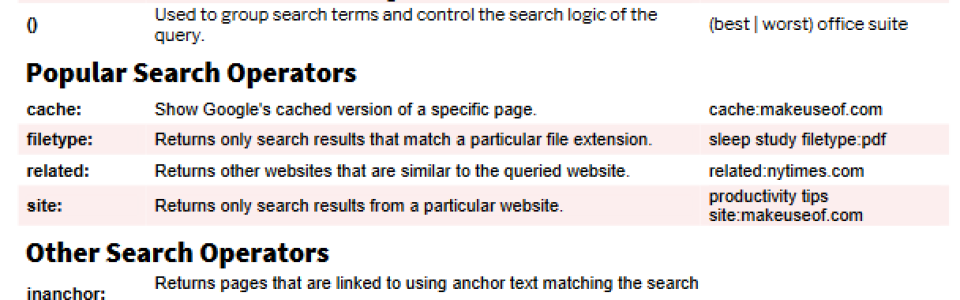
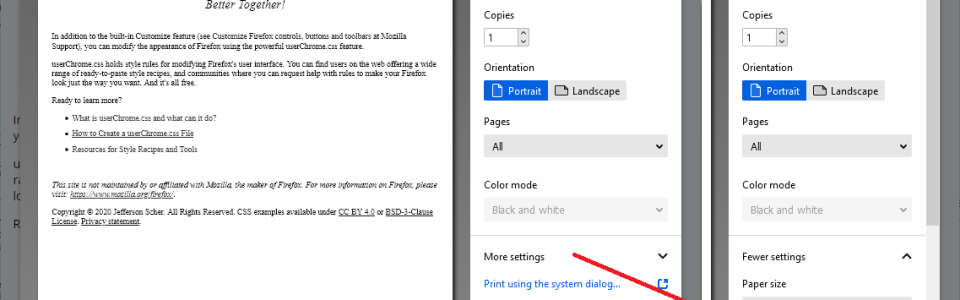
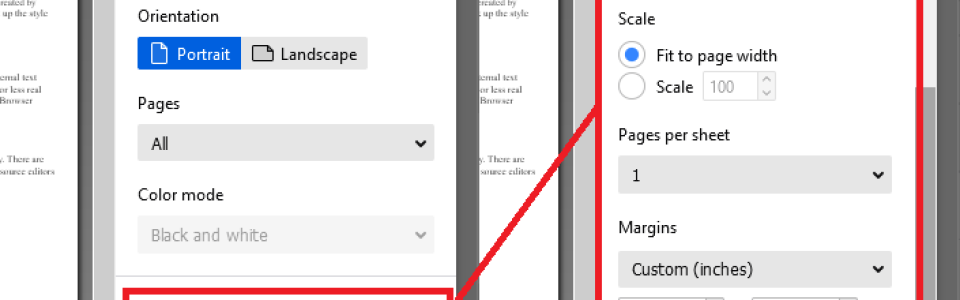
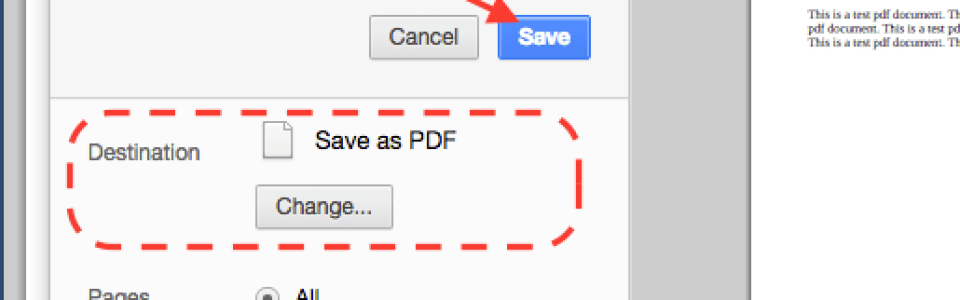
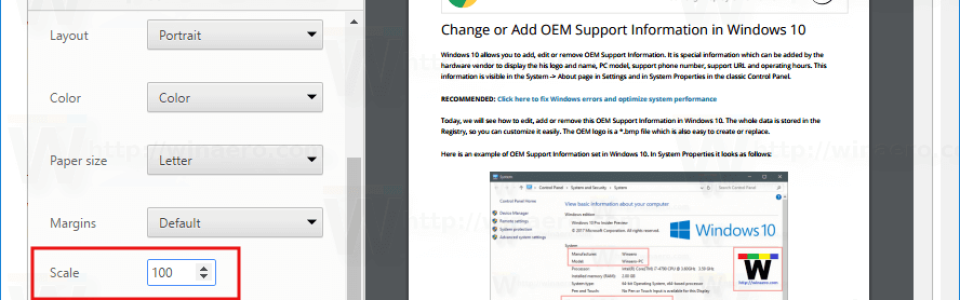

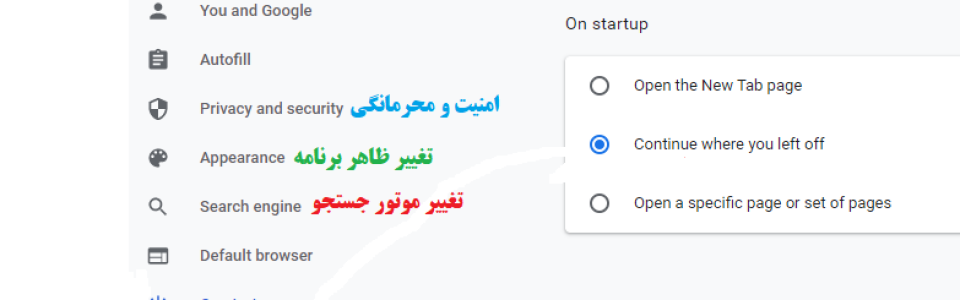
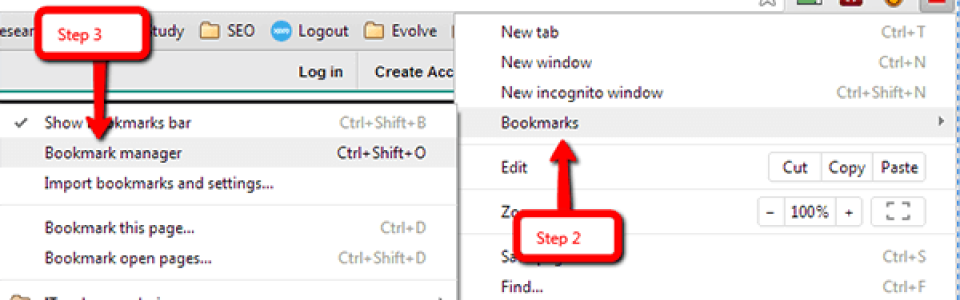
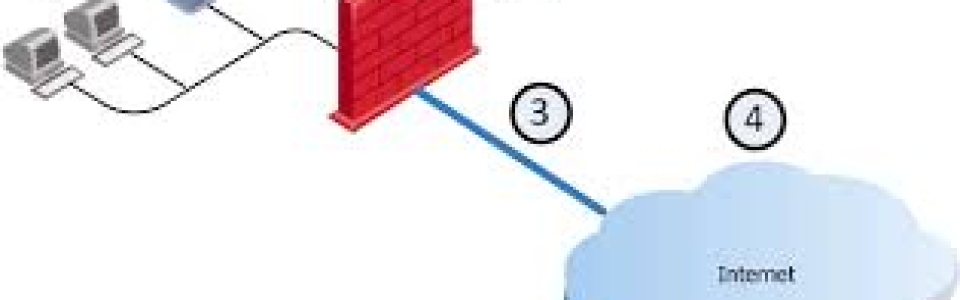

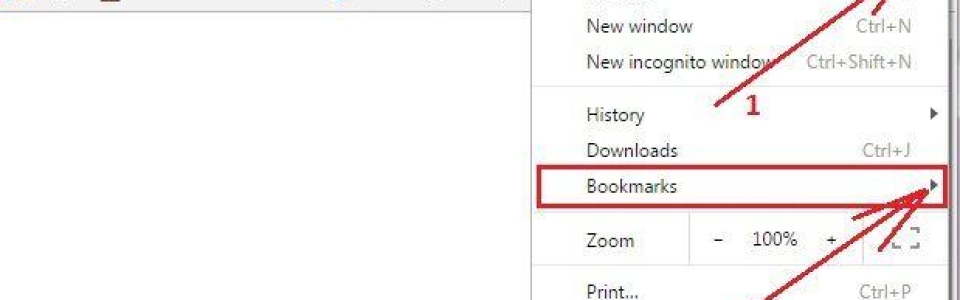


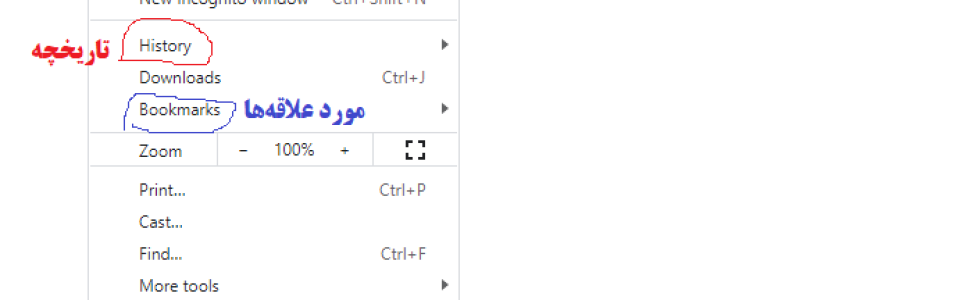
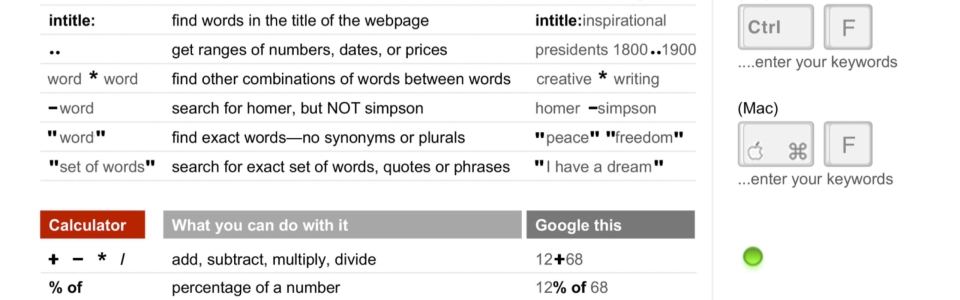


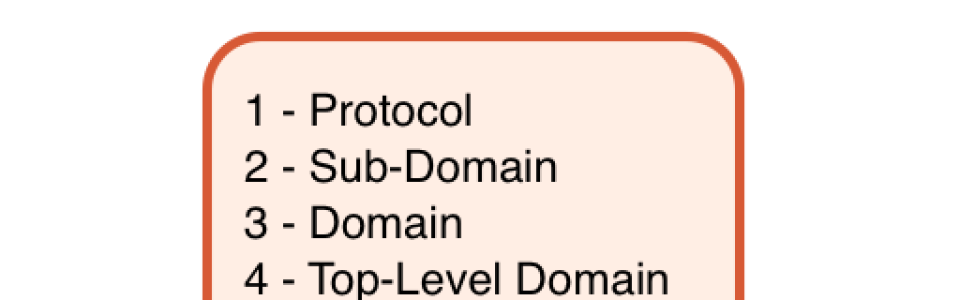
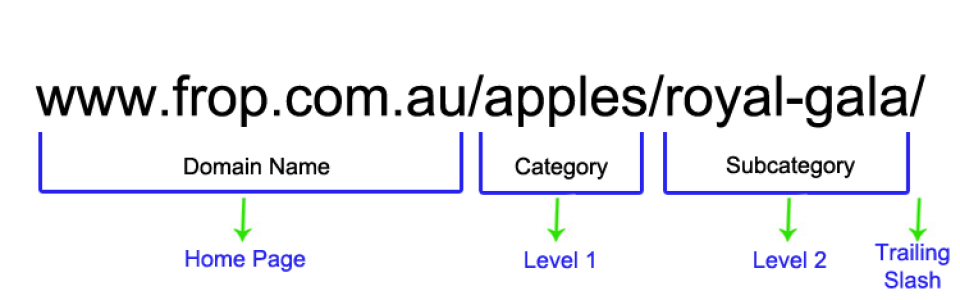
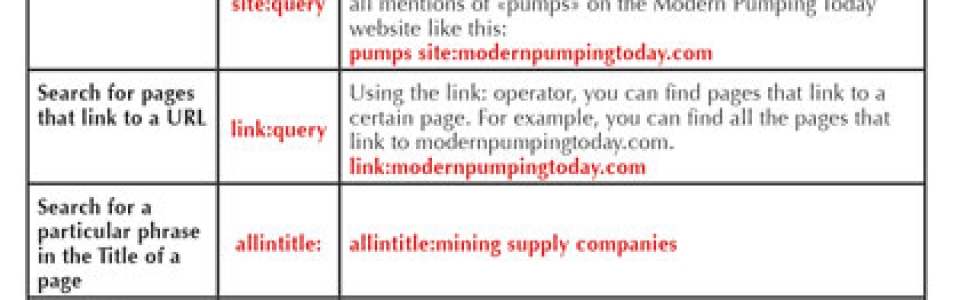

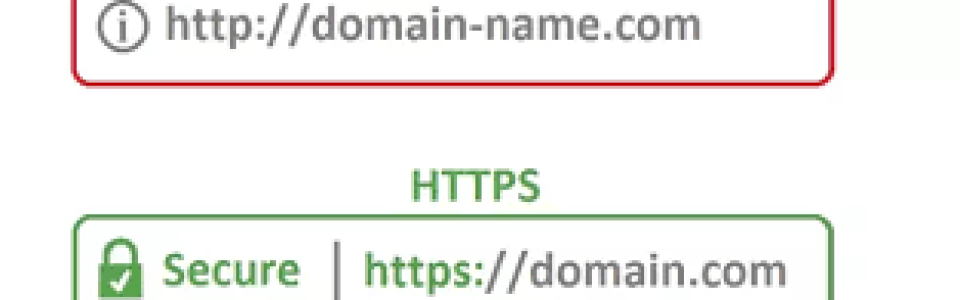
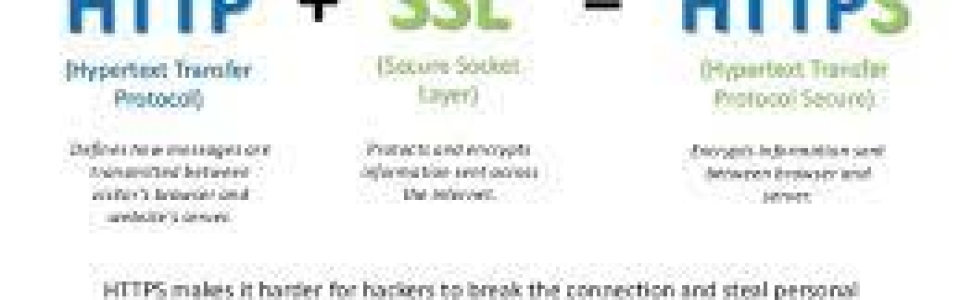
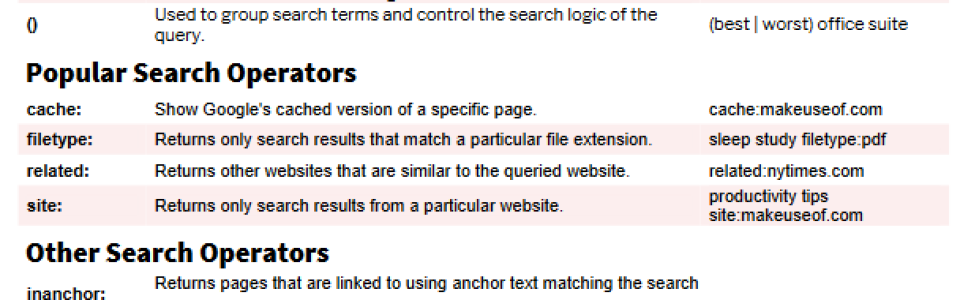
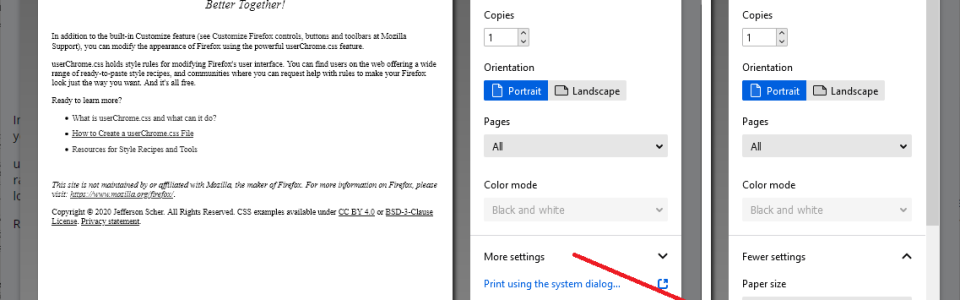
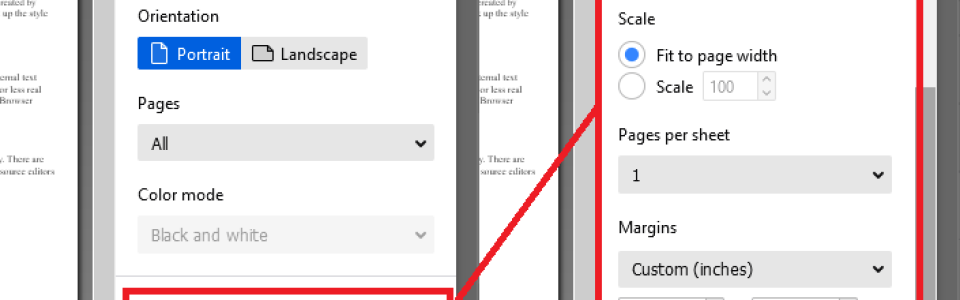
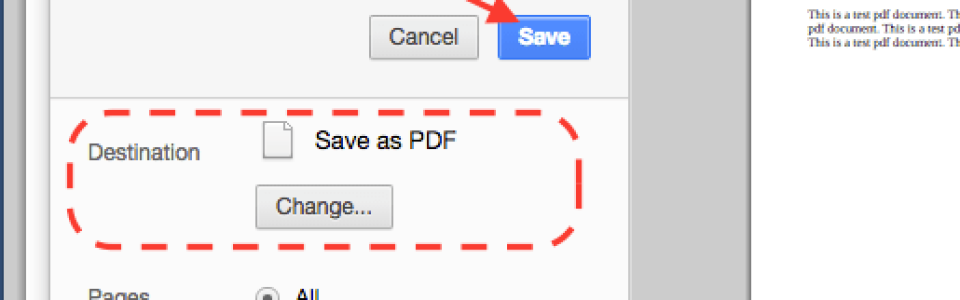





![AI-powered healthcare, with Archie Mayani [Video]](https://www.aiacceleratorinstitute.com/content/images/2025/08/Archie-Mayani.png)


